Hussain Varawalla – Healthcare Architect
Thirty-Five years of experience in the conceptualization and schematic design of medium to large health care facilities / hospitals in India.

(Completed 28/32 credits towards)Master of Architecture Kent State University, Kent, Ohio, USA
450-Bed Central Accident & Trauma System, New Delhi
Thesis project, Kent State University, Kent, Ohio -1989
Bachelor of Architecture (Hons) Indian Institute of Technology,
Kharagpur, West Bengal, India.
250-Bed Multi-Specialty Hospital at Mahim, Mumbai
Thesis project, Indian Institute of Technology, Kharagpur-1979
(With COVID-19 Lockdown Hair)( Me with my beloved sister and my books)


Employment Record
| Name of the Firm | Position Held | Years of Employment |
|---|---|---|
| Healthcare Architecture | Principal Consultant | Six |
| Hosmac India Private Limited | Mentor-Design Services | Three |
| Reliance Health Ventures Ltd. | Consultant-Architecture | Two |
| Hosmac India Private Limited,Mumbai | Director-Design | Ten |
| Asian Health Services, Bangalore | GM Architecture | Two |
| Indian Hospital Corporation, Chennai | Mngr.-Architecture | Two |
| HFP/Alan Ambuske, Cleveland, Ohio | Architect (USA Trainee) | One |
| Bharat Kothari & Associates, Mumbai | Architect | Four |
| Vijay Raheja & Associates, Mumbai | Architect | Five |
| Uttam C. Jain-Architect, Mumbai | Architect | Four |
| I. M. Kadri – Architect | Trainee | SixMonths |
Dedicated Healthcare Architectural Firms in Red
Did Healthcare work too in these architectural firms
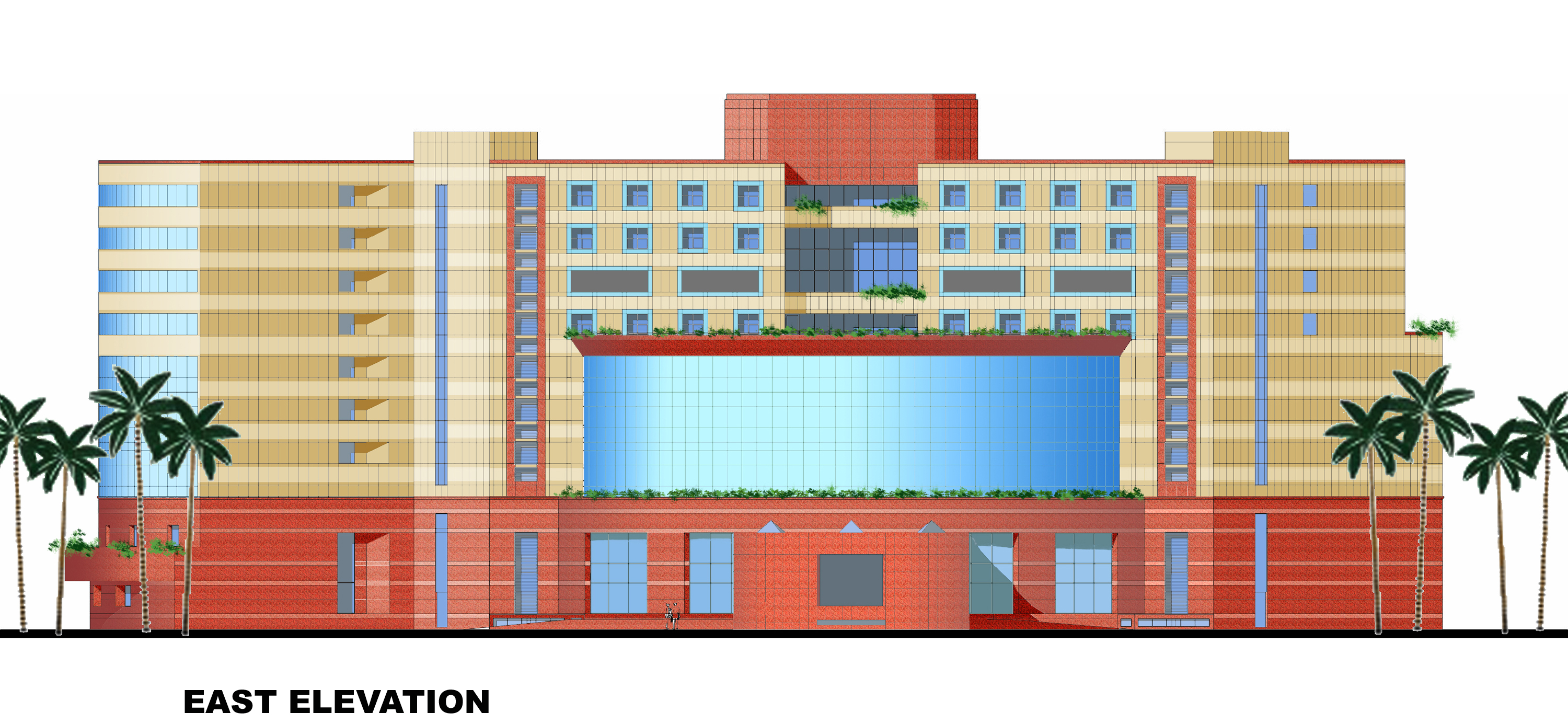
Asian Heart Institute – Bandra-Kurla Complex, Mumbai
“Mumbai’s renowned Asian Heart Institute (AHI) has been ranked by an international organisation the “safest cardiac hospital in the world” with the lowest mortality rate, a hospital official said Friday. AHI’s vice chairman and managing director Ramakant Panda said the hospital was accorded the honour among 15 hospitals in eight countries that participated in the International Cardiac Benchmarking survey conducted by the Joint Commission International (JCI). “This included data analysis of more than 6000 cardiac surgeries between October 2009-March 2011,” Panda told IANS here. The 15 JCI accredited hospitals had to provide data captured on a daily basis on the surgeries conducted and reported, set parameters to measure the quality of care provided and cooperate with verification visits by principals, said Panda, who performed heart surgery on Prime Minister Manmohan Singh nearly three years ago. “After the detailed three-year study, AHI has ranked No.1 in terms of ‘lowest complication rates’ and ‘highest survival rates’ as per the JCI survey,” he said.”I am proud to have been the designer of this outstanding hospital. What made it possible was an outstanding, visionary client.
Scope of Work – Hussain Varawalla
Healthcare Facility Planner
ARCHITECTURAL PROGRAMMING
The architectural space program consists of a list of the number and type of hospital beds proposed, and the different types of hospital departments further broken down into individual rooms with their areas and numbers.
At the end of the list of rooms in each department, there is a conversion factor, varying from 20 to 35 per cent, to account for the horizontal circulation area or area of corridors. This percentage factor is based on the major circulation corridors having a clear width of 2.40 M (8’-0”), the international norm.
At the end of the list of departments, an additional factor is used to estimate the overall size of the hospital, to account for vertical circulation areas (such as staircases and elevators) and sometimes mechanical spaces to be provided on the floor.
It should be noted that these factors do not account for unique design features such as atriums and courtyards. Ultimately, the actual design will determine the final space requirements.
It is important to always define and understand how square feet/square meters are calculated. Misunderstandings among members of the planning team can be disastrous since the gross space requirement is substantially higher than the net space requirement, because of the multiplier factors discussed above.
HEALTHCARE ARCHITECTURE ADVISORY SERVICES
If you should so desire, I can work in collaboration with another healthcare architect of your choice. The scope of work can be decided by discussion between the three of us.
I can, if wanted to, suggest appropriate honest and competent healthcare architects who can work in collaboration with me, for you to choose from.
I can also help you to choose an appropriate parcel of land for the site of the proposed hospital by analyzing its suitability to house the requirements of the proposed project. Speaking from experience, this can be a very cost-effective exercise. Many clients have come to me with completely unsuitable sites, sometimes bought at considerable cost, which defeats the very purpose of the whole design exercise right from the beginning. A little thought given to this aspect of the project at the onset can go a long way to making the project financially feasible and operationally efficient.
The land acquisition process, at a minimum, must involve consideration of the following factors:
1. Size of land. Make sure that the land is large enough to meet long-range growth plans – that is, a 10-year to 20-year growth plan.
2. Usable land. Determine the total acreage that can be used. The total size purchased is rarely the same as the total acres available for the actual building.
3. Zoning restrictions. Be aware of the current zoning limitations and allowances for the area.
4. Potential adjacent development. Find out what businesses and developments are planned or permissible in the adjacent spaces. Those potential developments might not be compatible to healthcare delivery.
5. Site access. Determine if the site is accessible through major roads and if it is fairly or highly visible to passers-by.
6. Services to the site. Evaluate the cost effectiveness of bringing service utilities to the site.
7. Preliminary master site plan. Prepare preliminary master site plans for each potential property. This plan ensures that all current planned facilities and their associated parking needs fit the property. Also, the potential property should have extra space for future development.
The key point to remember here is to never let the land drive the design of the facility.
“If you don’t know where you’re going, any path will take you there.”
Sioux Proverb
“Long-range planning does not deal with future decisions, but with the future of present decisions.”
Peter F. Drucker (1974)
“Intelligent people do not make important decisions on matters about which they are ignorant when additional data are easily available.”
John Kay & Mervyn King: “Radical Uncertainty: Decision –making for an unknowable future”
There is no single right answer or path forward, but there is one right way to frame the problem.
Clayton Christensen, Professor – Harvard Business School
These three lessons – take robustly good actions, build up options, and learn more – can help guide us in our attempts to positively influence the long term
William MacAskill – What We Owe the Future
No human purpose achieves dignity until it can be called work, and when you can experience a physical loneliness for the tools of your trade, you see that the other things – the experiments, the irrelevant vocations, the vanities you used to hold – were false to you.
Beryl Markham – West with the Night
If you want to have good ideas, you must have many ideas
Linus Pauling – Nobel Prize Winner in Chemistry, 1954
As more data becomes available and as the economy continues to change, the ability to ask the right questions will become even more vital. No matter how bright the light is, you won’t find your keys by searching under a lamppost if that’s not where you lost them. We must think hard about what it is we really value, what we want more of, and what we want less of.
Erik Brynjolfsson & Andrew McAfee – The Second Machine Age: Work, progress and prosperity in a time of brilliant technologies
“In a way, I like this phase of a novel better than the actual writing of it. In the beginning, there are so many possibilities. With each detail you choose, with every word you commit yourself to, your options close down.”
John Irving: “A Widow for One Year”
“CDS (Chief of Defence Staff) Chauhan is in regular touch with the three service chiefs to work out solutions to obstacles that they are likely to encounter in implementing this immense paradigm shift. Indeed, the armed force will have to usher in momentous changes in the way operations, logistics and application of force will be handled under theatre commands.‘The start of this journey depends on right first steps being taken towards jointness and integration,’ Gen. Chauhan has said.”
Pradip R. Sagar – Strength In Unity – India Today – August 21, 2023
Well said! The start of any journey (or project) depends on taking the right first step. If you start off in the wrong direction, you will never arrive at the right destination, no matter the amount of effort you put into it. Beginnings are very important.
“I think you learn more if you’re laughing at the same time.”
Mary-Ann Shaffer and Annie Barrows – The Guernsey Literary & Potato Peel Pie Society.
“The significant problems we face cannot be solved by the same level of thinking that created them.”
Albert Einstein
“A problem well stated is a problem half solved.”
Charles F. Kettering – American inventor
“To act only when a problem becomes obvious is to miss an important opportunity to solve the problem.”
Donella H. Meadows – Thinking in Systems
“The Earth is our Mother. She nourishes us. That which we put into the ground she returns to us.”
Big Thunder (Bedagi) Wabanaki Algonquin
“For every complex problem there is an answer that is clear, simple and wrong”
H.L.Mencken – Journalist and Essayist
“We are free to do what we want as long as it is what everyone else is doing and what our political and economic system expects us to do.”
Thomas Fisher – Philosopher and Architect
“Manifest plainness, embrace simplicity, reduce selfishness, have few desires”
Lao-Tzu
“It is better to conquer yourself than to win a thousand battles”
Gautama Buddha
“The highest activity a human being can attain is learning for understanding, because to understand is to be free”
Benedict de Spinoza
“The degree of one’s emotions varies inversely with one’s knowledge of the facts”
Bertrand Russell
“The intellect of man is forced to choose
Perfection of the life, or of the work,
And if it takes the second must refuse
A heavenly mansion, raging in the dark.”
William Yeats, “The Choice”
I have seen nothing, understood nothing,
Lord, help me see, make me understand.”
Rajanikanta Sen –Bengali Poet and Composer
“Some people like to muse on the philosophical conundrum ‘What is the meaning of life?’ But more practical philosophers ask, ’How can I make my life meaningful?’ The happiest people in the world ask, ’What if I could find some way to get paid for doing what I love?’”
Michael J. Gelb – Think Like Da Vinci
“Such bribyng for the purse, which ever gapes for more,
Such hordyng up of worldly wealth, such keeping much in store…
Such falshed undercraft, and such unstedfast ways,
Was never sene within men’s hartes, as is found nowadays.”
Anonymous
“If the only tool you have is a hammer, you tend to see every problem as a nail.”
Abraham Maslow – American psychologist
“She seemed so content and happy that I felt bound to ask: ‘So this is your Shangri-La?’
She thought about this for a bit. ‘There are many challenges here, of course,’ she said, ‘but most of them are in your mind – and if a place can help you see that, then what else is it but Shangri-La?’”
Amitav Ghosh – Wild Fictions
‘What we need to become happier and to make the world a better place is not more pious illusions but a clearer understanding of the way things are.
The mere fact that you have the leisure to read this book puts you in very rarefied company. Many people on earth at this moment can’t even imagine the freedom that you currently take for granted.”
Sam Harris – Waking Up
We have to look far in the distance when we try to put right what is wrong at the moment. We should worry about what new problems we create when we try to solve a problem…
Abdulrazak Gurnah – The Last Gift
Endure. A word as solid as a tree trunk. A good word upon which to build a life, I thought. I would learn it, and it would help me through dark times.
…I pondered the word endure, what it meant. It didn’t mean giving in. It didn’t mean being weak or accepting injustice. It meant taking the challenges thrown at us and dealing with them as intelligently as we knew until we grew stronger than them.
…the more love we distribute, the more it grows, coming back to us from unexpected sources. And its corollary: when we demand love, believing it to be our right, it shrivels, leaving only resentment behind.
…such is the paradoxical power of the mind. When we control it, it’s our best friend, but when we allow it to control us, it becomes our worst enemy.
Chitra Banerjee Divakaruni – The Forest Of Enchantment
The love of God can’t fill an empty belly and when it’s full one seldom thinks to thank Him.
On a single bush one is constantly surprised by the remarkable character shown by each individual rose. But from the house all one sees is a garden, which is all there is to it anyway in the long run.
Paul Scott – The Towers of Silence
Men are disturbed not by things, but by the view they take of them.
Epictetus – A Stoic Greek philosopher
…one of the truly bad effects of religion is that it teaches us that it is a virtue to be satisfied with not understanding.
Richard Hawkings – The God Delusion
A selfish hand has a short reach.
Hernan Diaz – Trust
I don’t believe in god…humanity is god. Humanity is the only god I know. If humanity doesn’t need something it will disappear. People who are not loved will disappear. Everything that is not loved will disappear from the face of the earth. We only exist through the love of others and that’s what it’s all about.
Peter Carey – Do You Love Me? – Collected Stories
But he would continuously change them around, according to his studies and tastes of the moment, for he considered books as rather like birds which it saddened him to see caged or motionless.
Italo Calvino – Baron In the Trees – Our Ancestors
Oh, my dear boy, one mustn’t expect gratitude. It’s a thing no one has a right to. After all, you do good because it gives you pleasure. It’s the purest form of happiness there is. To expect thanks is really asking too much. If you get it, well, it’s like a bonus on shares on which you’ve already received a dividend; it’s grand, but you mustn’t look upon it as your due.
W. Somerset Maugham – The Back Of Beyond – Collected Short Stories – Volume 4
Happiness is when what you think, what you say, and what you do are in harmony.
Mahatma Gandhi
Words are like birds…When you publish books, you are setting caged birds free. They can go wherever they please. They can fly over the highest walls and across vast distances, settling in the mansions of the gentry, in farmsteads and labourer’s cottages alike. You never know whom those words will reach, whose hearts will succumb to their sweet songs.
More and more, he comes to realize that people fall into three camps: those who hardly, if ever, see beauty, even when it strikes them between the eyes; those who recognize it only when it is made apparent to them; and those rare souls who find beauty wherever they turn, even in the most unexpected places.
Have I told you the story of Ibrahim? I don’t think so. Well, Ibrahim was God’s beloved. That is why Nemrud hated him. He said to his henchmen: build a fire, cast Ibrahim into it…He was cruel. But it is also important to ask how everyone else behaved when calamity struck. Many just watched. Some even rushed to fetch wood, to add to the blaze. The lizard, for instance. Only a few good souls tried to save Ibrahim – like the frog. It filled its mouth with water and spat into the flames, and kept doing this, until it was exhausted. The lizard laughed and said, “You are tiny, the fire is massive, what do you think you’ll achieve with your itty-bitty water?” But the frog said “If I were to do nothing, would I be any different from you?”
Clock-time, however punctual it may purport to be, is distorted and deceptive. It runs under the illusion that everything is moving steadily forward, and the future therefore, will always be better than the past. Story-time understands the fragility of peace, the fickleness of circumstances, the dangers lurking in the night but also appreciates small acts of kindness. That is why minorities do not live in clock-time. They live in story-time.
You can be our guest for as long as you’d like. That is…very generous of you…I would not want to be a burden. Not a burden…We believe an onion shared with guests tastes better than roast lamb.
Elif Shafak – There Are Rivers in The Sky
You have to get out of your own way.
Henry Winkler – Actor, producer, director, author
“A situation in itself,” he said, “is neither happy nor unhappy. It’s only your response to it that causes your sorrow. But enough of philosophy! I’m hungry.”
Chitra Banerjee Divakaruni – The Palace of Illusions
Didn’t you tell me this past week one of the things you loved was bees and honey? Now, if that’s so, you’ll be a fine beekeeper. Actually, you can be bad at something…but if you love doing it, that will be enough
Sue Monk Kidd – The Secret Life Of Bees
Nobody made a greater mistake than he who did nothing because he could only do a little.
Edmund Burke – Philosopher
It is seldom very hard to do one’s duty when one knows what it is, but it is often exceedingly difficult to find this out.
Samuel Butler – English novelist and critic
“Man did not weave the web of life, he is merely a strand in it. Whatever he does to the web, he does to himself.”
Chief Si’ahl (Seattle) (1780-1866) – Chief of the Duwamish and Suquamish tribes
“…doing what the person paying the fees wants has come to trump personal reservations of most professionals, turning us into what philosopher Thomas Hobbes called “artificial persons, in which we set aside our own scruples to serve our clients.
This raises a question about the ethics of service. How much does our duty extend beyond meeting clients’ programs to helping them see their wishes in a larger context and their short-term requirements over the long term? Immanuel Kant’s duty ethics helps us answer such a question. He would argue that an ethical person – and I would add, an ethical professional – does what is right when viewed in the largest scale and what reason requires, regardless of the possible awkwardness of countering a client’s intentions. We should do so not because it might make us feel less artificial but because it serves clients’ real interests, whether they see it that way or not.
For clients who request things that may lead to their ruin, the professional has a duty to explain the consequence of that request, the calamity that lavish desires can cause, as Lao tzu put it. And if clients refuse to listen, we need to be ready to refuse the requests we think ill advised. That can, of course, lead to our dismissal, but this broader sense of advice also preserves what it means to be a professional: we should not do for others that which we would not do ourselves.”
Thomas Fisher – Ethics for Architects – Self Destructive Behavior
“I do not ask your absolution. I simply ask you to see that there is only one thing to do when we fall, and that is to get up, and go on with the life that is set in front of us, and try to do the good of which our hands are capable of for the people who come in our way.”
Geraldine Brooks – March
“Do you think you are doing God’s work?” (she) asks her. “Because I know that God’s work is not done through prayers and not through kissing hands. You have to get your hands dirty.”
Mohammed Hanif – Our Lady of Alice Bhatti
“Weather was often blamed for Africa’s troubles, but “what is the use of ascribing any catastrophe to nature?” Rebecca west asked herself in ‘Black Lamb and Grey Falcon’, and answered, “Nearly always man’s inherent malignity comes and uses the opportunities it offers to create a graver catastrophe.”
Paul Theroux – The Last Train to Zona Verde
“He drank an expresso macchiato and ate a croissant at a counter from where he watched the workers hurrying to and from their jobs, and he had a long overdue insight. He understood that leisure was the most expensive commodity on the planet, so rare a thing that the wealthy could not afford it. No one could, except the homeless and the deranged.”
Jeet Thayil – The Book of Chocolate Saints
“Humour can get in under the door, while seriousness is still fumbling at the handle.”
GK Chesterton
“If thou suffer injustice, console thyself: the true unhappiness is in doing it.”
Democritus
“Take care of those who work for you and you’ll float to greatness on their achievements.”
H. S. M. Burns
“He might…demonstrate in his own lifestyle, how others can live with much less and still live well. And in doing so, he would reveal the ancient maxim at the core of sustainability: that a good life for all involves freeing ourselves from insatiable desires and finding happiness in living with what we absolutely need, to ensure that those who follow us have the same opportunity”
Thomas Fisher – Ethics For Architects
“Always design a thing by considering it in its next largest context – a chair in a room, a room in a house, a house in an environment, an environment in a city plan.”
Eliel Saarinen
“We think sometimes that poverty is only being hungry, naked and homeless. The poverty of being unwanted, unloved, and uncared for is the greatest poverty.”
Mother Teresa
“People think there are answers to the world’s problems’, he said, … ‘But there aren’t any answers because the world’s fundamental problem is that most people are stupid. Never mind that they don’t buy art and don’t read books and don’t think for themselves – that’s a given…it’s another kind of stupidity – animal stupidity. Dumb instinct. People make the same fatal mistakes every generation – in war, in politics, in business. The history of the world is the history of human folly. Nothing will change.Everything gets worse.’”
Paul Theroux – The Vanishing Point – The Vanishing Point
“This is what I meant when I said the atheistic worldview requires intellectual courage. It requires moral courage, too. As an atheist, you abandon your imaginary friend, you forgo the comforting props of a celestial father figure to bail you out of trouble. You are going to die, and you’ll never see your dead loved ones again. There’s no holy book to tell you what to do, tell you what’s right or wrong. You are an intellectual adult. You must face up to life, to moral decisions. But there is dignity in that grown-up courage. You stand tall and face into keen wind of reality. You have company: warm, human arms around you, and a legacy of culture which has built up not only scientific knowledge and the material comforts that applied science brings but also art, music, the rule of law, and civilized discourse on morals. Morality and standards for life can be built up by intelligent design – design by real, intelligent humans who actually exist. Atheists have the intellectual courage to accept reality for what it is: wonderfully and shockingly explicable. As an atheist, you have the moral courage to live to the full the only life you’re ever going to get: to fully understand reality, rejoice in it, and do your best finally to leave it better than you found it.”
Richard Dawkins – The Hubris of Religion – The Four Horsemen.
“Odoric’s story bears out the idea that at the end of our exploring we arrive where we started, but we understand that starting point anew. On returning from their journey, the traveller is somehow changed, wise in new ways, having encountered radical difference and wonderful similarity, their home life and prior knowledge thrown into a new relief. Travel forces us to consider the significance of our lives, and to encounter the littleness of the human amid the planet’s variety and unknowability.
As he struggled homewards, the dying Odoric may well have felt that the earth he had traversed had itself become tiny, nothing more than a series of points on a small surface, and that the time had come to turn from earthly things to the celestial. This was not to cease roaming, but to search instead for yet other worlds. As the sun set and the blue deepened into night, Odoric received his passport into the skies, to join those released from their bodies and from earthly travels, into the brilliant circles amid the blazing stars where the soul would begin its mysterious, incorporeal journey towards the horizon of infinity.”
Anthony Bale – A Travel Guide To The Middle Ages: The World Through Medieval Eyes
“If our society were truly to appreciate the significance of children’s emotional ties throughout the first years of life, it would no longer tolerate children growing up, or parents having to struggle, in situations that cannot possibly nourish healthy growth.”
Stanley Greenspan, MD – The Growth of the Mind
“Thus, in his case, no more hoping that he would become normal again. That he would live a normal life. That what had happened would not have happened. Forget all that. Therapy taught him to give up those hopes. Hope would have to reside in something like this: hope to do some good, no matter how fucked up you are. This was worth writing down on a piece of paper, in shaky block lettering, and then pinning the paper onto the mirror in his bathroom, along with various other encouragements in the form of phrases or images, probably it looked like a madman’s mirror, but he wanted to put things up there HOPE TO DO SOME GOOD, NO MATTER HOW FUCKED UP YOU ARE.
“The whole field and discipline of economics, by which we plan and justify what we do as a society, is simply riddled with absences, contradictions, logical flaws, and most important of all, false axioms and false goals. We must fix that if we can. It would require going deep and restructuring that entire field of thought. If economics is a method for optimizing various objective functions subject to constraints, then the focus of change would need to look again at those “objective functions.” Not profit, but biosphere health, should be the function solved for; and this would change many things. It means moving the enquiry from economics to political economy, but that would be the necessary step to get the economics right. Why do we do things? What do we want? What would be fair? How can we best arrange our lives together on this planet?
Our current economics has not yet answered any of these questions. But why should it? Do you ask your calculator what to do with your life? No. You have to figure that out yourself.
Kim Stanley Robinson – The Ministry for The Future
“(She) held out her hand and he squeezed it with his left one. Then she noticed that he was missing several fingers on his right hand, but he explained that he could play the guitar anyway, because there is always a way to do what you want to do.”
“In almost every family there’s a fool or a crazy person,” (she) assured her while she concentrated on her knitting…” You can’t always see them, because they’re kept out of sight as if they were something to be ashamed of. They’re locked up in the back room so visitors won’t see them. But actually there’s nothing to be ashamed of. They’re God’s creatures too
Isabel Allende – The House of The Spirits
“The bureaucrats would bring the hammer down on the silliest, most light-hearted things. For example, they objected to a scene in which a somewhat irreverent French tourist dips his samosa in bright green coriander chutney, smiles at the other guest at the table and says, in French-accented English, ‘You know, in Eendia, every day my shit is a different colour.’”
Arundhati Roy – Mother Mary Comes To Me
“For what matters in life is not whether we receive a round of applause; what matters is whether we have the courage to venture forth despite the uncertainty of acclaim.”
Amor Towles – A Gentleman in Moscow
“The eye of the true artist doesn’t see life in the way of goods paid for. The world is ours. It is our birth-right. We take it without payment.”
Muriel Spark – The Complete Short Stories – The Fathers’ Daughters
“Our job is to give the client, on time and on cost, not what he wants, but what he never dreamed he wanted; and when he gets it, he recognizes it as something he wanted all the time.”
Denys Lasdun, architect
Perhaps it seems arrogant for the architect Denys Lasdun to make the above statement. But I think that we should try to see through the apparent arrogance of the statement, to the underlying truth that clients do want designers to transcend the obvious and the mundane, and to produce proposals that are exciting and stimulating as well as practical. What this means is that designing is not a search for the optimum solution to the given problem, but that it is an exploratory process. The creative designer interprets the design brief not as a specification for a solution, but as a starting point for a journey of exploration; the designer sets off to explore, to discover something new, rather than to reach somewhere already known, or to return with yet another example of the already familiar.
Important Design Factors Healthcare Facility Planning
Following are important design factors to be considered in your design approach:
- Freshness and Originality in the Design Approach – A Different Mindset – no baggage carried forward from past projects
- Sustainability – Green Building Rating – Low Carbon Footprint – Hippocratic Oath: “First, Do No Harm” – focus also on IAQ (indoor air quality)-no outgassing of VOC’s (volatile organic chemicals) which can be toxic and create “sick building syndrome”.
- Flexibility of the Design to Accommodate Future Requirements – Ease of making Changes over Time – Reserved Rights of Way for Service Runs – Separation of the Structure from the Planning – Design the Basic Structure for a 100 Year Life – Primary System: RCC structure, column grid 8.4 x 8.4 M to 9.1 x 9.1 M as per current Western hospitals – built to last 100 years. Secondary system: walls and MEP – built to change after 25 years as and where necessary. Tertiary System: FF&E – furniture, fixtures and equipment – change even in the short run. Systems Separation.
- Bringing Nature into the Building – Views of Nature – Terrace Gardens – proven fact that it enhances patient recovery
- Natural Light and Ventilation as a Design Factor – light wells, courtyards, alphabet architecture?
- Energy Efficient Design – MEP design, passive solar
- Climate Change and Extreme Weather Events Resilient Design – eliminate expensive equipment in basements? Overdesign HVAC cooling systems by 20% to cope with heat waves and future increased AC load?
- Ease of Wayfinding by Design for Patients Under Stressful Mindsets – colour coding floors, supergraphics, views to the outside to help orientation within the building
- Use of Colour and Artwork in Interior Spaces – see above. Artworks as events marking where you are, help in orientation
- Patient Centric Design – A Hospital beyond “A Doctor’s Workshop” – keep the well-being of the patient and visitor uppermost
- Therapeutic Rooftop Garden – museum of medicinal plants
- Water Conservation – Efficient Fixtures – rainwater harvesting
- Optimised HVAC Design – overdesign to take care of future unanticipated AC load during heat waves?
- Passive Solar Features – Sun Shading Devices – Corbusier’s brise soliel
- Evidence Based Design – Using Environment Behaviour Studies – a scientific basis for taking design decisions
- “At the Beginning of a Project the Big Decisions Get Made” – The Importance of Strong Conceptual Design
- Use of Design Charrettes to Determine Real Needs – Participation of Staff/Doctors in Conceptual Design – get staff/doctors buy-in into the design by hearing them out and responding to their comments
Specialized Hospitals: Design and Planning
Edited by Rebel RobertsThe Healing Wheel of the Environment
By Tom Danielsen
“The effect in sickness of beautiful objects, of variety of objects and especially of brilliancy of colours is hardly at all appreciated. People say the effect is only on the mind. It is no such thing. The effect is on the body too. Little as we know about the way in which we are affected by form, by colour and light, we do know this, that they have an actual physical effect. Variety of form and brilliancy of colour in the objects presented to patients is an actual means of recovery.” Florence Nightingale, 1885.

Evidence-Based Design
Internationally, there is an increasing focus on Healing Architecture and Evidence-Based Design (EBD). EBD is seen as a parallel to evidence-based medicine, and is defined as “the deliberate attempt to base design decisions on the best available research evidence…Evidence-based healthcare designs are used to create environments that are therapeutic, supportive of family involvement, efficient for staff performance, and restorative for workers under stress. An evidence-based designer, together with an informed client, makes decisions based on the best information available from research and project evaluations.” Hamilton DK (2003) The Four Levels of Evidence -Based Practice. Healthcare Design, November 2003.
Evidence-Based Design and the Healing Wheel of the Environment
On the basis of EBD, the DNU consultant group has developed “The Healing Wheel of the Environment”, which forms the planning foundation for the entire project. As EBD is a relatively new discipline, and limited in many respects in its scientific foundation, the logical consequence is that only “evident” areas are included in the wheel, which can be extended at any time. The twelve components of the Healing Wheel of the Environment are:
- Empowerment and ergonomics
- Daylight
- Single-bed rooms
- Acoustics
- Artificial light
- Access to the landscape
- Communication and logistics
- Textures
- Indoor climate
- Art
- IT
- Design and décor
Empowerment and Ergonomics
The patient must as far as possible be able to regulate the light, heating and music in the patient room. Via bedside PCs, patients will have access to their own journals and will be able to see the times of planned examinations, test results, etc. Improved ergonomic design will help to ensure less fatigue and stress.
Daylight
Daylight is not just important for our sense of well-being, but also for our health. Daylight helps to ensure that our circadian rhythms are correctly adjusted; it also lifts the general atmosphere, and has an anti-depressant effect. Patients in rooms will windows, particularly windows with green landscapes outside, have shorter periods of convalescence and fewer complications, and require less pain-relieving medicine. Careful and early planning of natural light can reinforce the positive effect of day light and help to prevent the problems that natural light can also cause, such as over-heating and dazzling. Besides improving personal comfort, the conscious use of daylight thus has both an environmental and an economic dimension.
Single-Bed Rooms
Research shows that single-bed rooms confer a number of benefits, including fewer hospital-acquired infections, fewer medication errors and a lower noise level. Single-bed rooms also mobilise the patients when they get up to eat, or meet other patients. They also provide privacy for conversations with hospital staff, and thereby a basis for better treatment. The arguments in favour of multiple bed rooms are usually that they are less expensive (to build and operate), but in fact the shorter periods of admission to hospital indicate that single-bed rooms are more economic from the point of view of society.
Acoustics
A room’s acoustic properties determine how sounds are disseminated there. The noise level of hospitals is notoriously high, with many simultaneous and different noise sources, such as people walking, talking or working, beep-sounds from equipment, and transportation noises – all in spaces with hard surfaces, due to cleaning requirements. A lower noise level can reduce stress for both patients and staff and help to give patients the peace and quiet they need. Good acoustic qualities contribute significantly towards a good indoor climate, and are best secured by selecting the right construction principles, an appropriate internal organisation and good surface materials.
Artificial Light
Artificial light must fulfil both functional and aesthetic needs. It must be flexible and variable and provide a sense of well-being, but must also be capable of being switched to diagnostic lighting, for example to examine changes in skin colouration. The choice of fittings and light sources must comply with both functional and atmospheric needs. Artificial light will be used in combination with daylight, and will take over the illumination function when daylight alone is insufficient.
Access to the Landscape
Patients must have access to gardens and landscaped areas. Nature has a positive effect on stress and fatigue, and its promotion of health and healing is well documented. Randomised studies have shown that a view of and access to natural surroundings can have a pain-relieving effect in itself. Gardens also cause patients to move around more, which has a positive effect on their healing, e.g. by encouraging the release of endorphins through exercise. They also provide suitable places to meet and talk with people.
Communication and Logistics
The New University Hospital in Aarhus is in dialogue with its surroundings: the existing hospital, the future new buildings and the landscaped environment. The hospital’s flow is clear, comprehensible and physically convenient for all user groups and staff. The hospital is built up around the large landscape garden, the Park, which is its most important physical landmark. The squares and arcades of the various blocks each have their own individual form and décor, and thereby their own identity. The building information will be supported by “speaking signs” – hand-held receivers which can read out signs and information boards in Danish, English, German or Spanish.
Textures/Surfaces
Surfaces influence and involve all of the senses. If we are to realise the vision of a clean, sensually rich, aesthetic, healthy and comfortable workplace, all of us – both the hospital, the occupational health services, organisations, researchers, advisers and public authorities – must work to promote a healthy working environment. All kinds of environmental factors should be given consideration in the project, and products with a positive effect on the indoor climate, including natural materials, should have preference. Efforts must be made to ensure that a large amount of the materials used can be recycled, and that the building materials are themselves based as far as far as possible on recycled materials. Partial or complete wood cladding should be used in some of the public areas, such as the Forum, arcades and squares.
Indoor Climate
The indoor climate of a building can influence a person’s health, well-being, quality of life and productivity. In a hospital building the patients are in a vulnerable health condition, and high productivity is expected of the staff. Accordingly, the indoor climate is of considerable importance to all who spend time there. The basic principle behind the maintenance of an optimum indoor climate is that the building and its physical qualities should enhance the indoor climate as far as possible. This is primarily done the use of heavy, well-insulated constructions and a combination of appropriate window areas, glass quality and sun screening to guard against over-heating or insufficient cooling. The building is then supplemented with technical installations such as heating and air conditioning equipment, which support the building’s physical qualities. This minimises dependence on the technical installations, which, besides conferring benefits in terms of energy use, ensures an optimum indoor thermal climate. In atmospheric terms, the ideal indoor climate is achieved by utilising materials which release no gases, or only release gases in tiny quantities, and via the use of filtered and conditioned air from outside.
Art
The other components in the Wheel are “rational and evident”. The rational and the irrational are inseparable; they define each other and are thereby interwoven. To meet art is to encounter something else. The appropriate relationship between the visual arts and architecture, and their modes of integration, is a perennial question. Art in the public arena offers free and enriching experiences. The construction of the New University Hospital Aarhus presents an exceptional opportunity to create original works in special places. By integrating art at as early a stage is possible, the patients, staff and visitors can be presented with larger and more complex works.
IT
The hospital of the future is a digital hospital. Wireless IT infrastructure is the natural starting point to enable both staff and patients to easily send and receive information in digital form. Pervasive computing can make health care independent of time and place, and can improve communication and coordination between the various levels of the health sector.
Design/Décor
In this context, design should primarily be understood as a combination of the traditional view of design and the modern perspective on design as a rational process of problem solving. At the New University Hospital design must contribute to improved solutions for staff, patients and relatives. The conscious use of well-designed, well-functioning products, furniture or fixtures brings benefits which extend beyond the immediate target group. Equipment design which combines advanced technology and attractive appearance with user-friendliness and good ergonomics will contribute to an improved working environment for the staff, with a reduced risk of operational errors and work-related injuries. A beautiful and friendly design without an overly mechanical appearance will also help to instil confidence and reassure nervous patients. In the same way, a well-designed patient room with a good décor and choice of materials will satisfy both the staff’s need for an efficient environment and the patient’s need for a friendly and confidence-inspiring space, in which elements from the domestic sphere help to call forth desirable associations and atmospheres, and in the final analysis contribute to more rapid healing and a shorter stay in hospital. The interior project, which encompasses both furniture and fixtures, must support and complement the overall vision of a modern, IT based and efficient hospital which focuses on the individual.
Wear The Old Coat, Buy The New Book
- It’s called reading, it’s how people install new hardware in their brains
- He said, “me or books?” I sometimes remember him when I buy new books
- In my dreams books are free and reading makes you thin
- Abibliophobia: Uh-bib-li-uh-fo-bee-uh Fear of running out of reading material
- The great thing about books is that there are no commercials
- I disappear into books. What’s your superpower?
- Booktrovert: A person who prefers the company of fictional characters to real people
- Books are a uniquely portable magic
- I am not addicted to reading. I can finish as soon as I finish the next chapter
- Anyone who has time to clean is not reading nearly enough
- Too many books? I think what you mean is not enough bookshelves
- That major sleep disorder you have is called reading
- Books are the very best defence against unwanted conversation
- My workout is reading in bed until my arms hurt
- A book commits suicide every time you watch a reality show
- Books are just TV for smart people
THE CHALLENGE OF PREDESIGN PLANNING
The planning and delivery of a major capital project can be divided into six stages, as shown in the figure below:
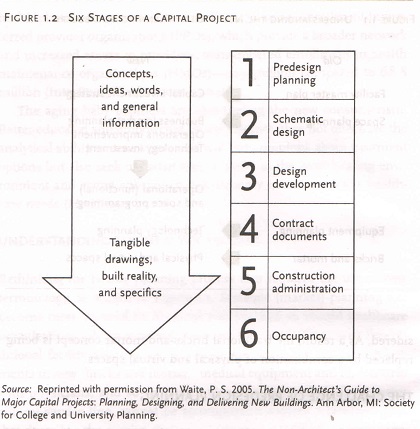
The first stage of predesign planning – the focus of this note – includes general concepts and ideas in the form of words, numbers and conceptual diagrams. Preliminary space estimates are used to develop a facility master plan and to generate project cost estimates early .Once specific projects are identified and approved, the detailed operational and space programming begins; when this is completed, the design architect can start the schematic design stage. Each subsequent phase brings more knowledge and detail about the project and has its own cast of players. Nearing the final phases, the concepts and ideas are translated into tangible architectural floor plans, drawings of construction details and the eventual reality of the three-dimensional building.
Predesign planning can be defined as the process of determining the following:
• Right services consistent with the organizations strategic initiatives, market dynamics, and business plan, at the
• Right size based on projected demand, staffing, equipment, technology, and desired amenities, in the
• Right location based on access, operational efficiency, and building suitability, with the
• Right financial structure – for example, owning leasing or partnering.
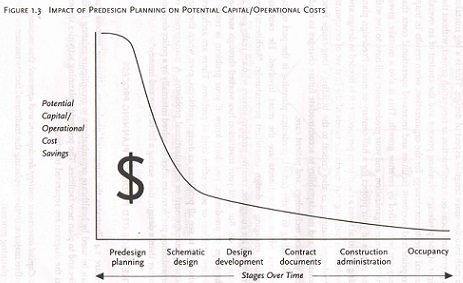
Predesign planning is the stage where the healthcare executive has the most influence on the potential success of the final project. His or her opportunity for input decreases as each subsequent stage passes. The opportunity to reduce both the initial capital cost and the ongoing operational costs is also greatest during the predesign planning stage, as shown in the figure below:
With the prospect of a new building project, healthcare executives tend to short-circuit or bypass the predesign stage to rush into the more tangible aspect of design. This is a big mistake. A premature focus on a construction or renovation project, without the rigor of a predesign planning process and the context of an overall capital investment strategy for the organization, often results in in inappropriate and overbuilt facilities and increased operational costs that may not be justified by revenue growth. This is also a mistake, given that you, your organization and your predecessors will have to live with the results of your project for half-century or more. Predesign planning is critical from a short term-term perspective: it is needed to design and construct a building that meets the needs of the first set of occupants. Predesign planning is also critical to the building’s long-range functional life and it’s adaptability to accommodate future changes in medical practice, technology, and patient care.
Predesign planning is the part of the process where non-architects are the most involved. There should be caution against engaging a design consultant prematurely. Architects and engineers are energetic, creative problem solvers who are really good at what they do. But until your institution has worked through some of the steps of predesign, you don’t know if your problem is really a design problem or some other kind of problem. There are architects who tend to see all problems as design problems, even when they’re actually management or organizational problems. A management or organizational problem can often be solved internally by a policy decision thus saving a lot of time and money.
THE INTEGRATED PREDESIGN PLANNING PROCESS
The figure below illustrates the integrated planning process that can be used by healthcare organizations to reconfigure existing facilities and to plan new facilities. The predesign planning activities shown in the diagram are separated into two:
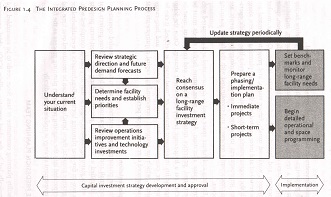
1. Capital investment strategy development and approval: this includes five major activities (replacing the traditional facility master planning process).
2. Implementation: this includes the detailed operational and space programming for designated projects and the establishment of benchmarks to monitor long-range facility needs as the strategy is periodically updated.
Capital Investment Strategy Development and Approval
The predesign process begins with the collection of baseline data and a review of the organizations current situation, including campus access and circulation, bed utilization and configuration, space allocation and layout, and infrastructure issues. Current market dynamics, workload trends, future vision and projected demand are also reviewed and incorporated into the facility planning process, along with the organizations institution-wide and service-line specific operations improvements initiatives. Planned technology investments are currently reviewed and coordinated with the facility planning process.
Existing and future space need is documented and compared with current space allocation. At this point, future facility needs must be determined, priorities must be established, and consensus must be reached on a long-range facility investment strategy. Once the long-range facility investment, or “road map”, is defined, it can be divided or categorized into immediate, short-term and long-range projects, which are assigned corresponding capital requirements that are sequenced over a multi-year period.
Implementation
With the phasing/implementation plan in hand, detailed operational (functional) and space programming can begin for those projects that are identified as immediate priorities, along with short-term projects for which planning needs to begin so that they can be completed in a two-to-five year planning horizon. Benchmarks are established for long-range projects; these benchmarks can be monitored over time and incorporated into the ongoing predesign planning process as the facility investment strategy is updated periodically.
This note on “Predesign Planning” has been adapted from the book “Healthcare Facility Planning: Thinking Strategically” by Cynthia Hayward, and is fully endorsed by me as relevant and necessary.
I encourage you to read this very good book; it is available on Amazon.in.
The Project Launch Phase
The following are key points to remember about the project launch phase:
• Spend sufficient time defining the scope, cost, and the schedule of the project.
• Develop a budget and schedule early.
• Complete the master facility plan and operational and space programming processes before entering the design phase.
• Make smart land-acquisition decisions. Acquire sufficient land to prevent the land from driving the design, to allow for future expansion, and to accommodate future changes in healthcare delivery and technology.
• Evaluate potential joint-venture opportunities and their impact on capital and operating cost.
• Assemble the key members of the project delivery team.
The Project Delivery Team
The following are key points to remember about the selection and organization of the project delivery team.
• Select external team members – project manager, lead architect, specialty consultants, and construction manager – during the launch phase.
• Organize the Facility planning Committee first. This committee should include representatives from the board and medical staff building committees.
• Identify people from the board, from medical staff, and from the community as “project champions” and involve them in the process.
• Select members for the departmental task forces, and then involve them in the development of the master facility plan, the Operational and Space Planning (O & SP) process, and the design phase. These forces should include physicians, staff, and volunteers from various departments.
• Base selection of key external staff members on qualifications, experience with similar projects, and chemistry with internal team members.
This note on “The Project Launch Phase” and “The Project Delivery Team” has been adapted from the book “Launching a Healthcare Capital Project” by John E. Kemper, and is fully endorsed by me as relevant and necessary.
I encourage you to read this very good book; it is available on Amazon.in.
Proposed 250-375 Beds Model Hospital
The Ability to Accommodate Change
Hospitals and large healthcare campuses need to be able to accommodate change. Buildings that cannot change, and especially healthcare buildings, which often remain in operation for 50-100 years or longer, are at risk of premature obsolescence. There are three ways in which buildings and building complexes can transform and accommodate changing needs: through flexibility, adaptability and expandability. Flexibility involves the ability of a given space, department, building or campus to accommodate changing needs with little or no physical reconfiguration. Adaptability involves planning and constructing buildings or building elements with the capability to transform space easily with the least amount of physical, material and economic impact. Expandability involves planning to accommodate growth and change in a coherent and logical way. It requires planning infrastructure and circulation in a way that anticipates future growth.
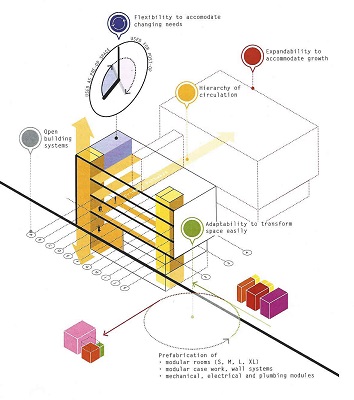
A change-ready hospital. Source: Heinle, Wischer and Partner
Primary Drivers
The healthcare context is incredibly dynamic and influenced by constant changes in medical science and technology, healthcare policy and regulations, demographic transformations in both populations served and caregivers, and evolving clinical practices and approaches. Collectively not only are these forces increasing in their impact but also the arte and pace of change are accelerating. Healthcare as delivered 50 years was fundamentally different than today. Facilities that were designed and built then and are still in use were not conceived to easily accommodate changing healthcare needs, practices, and technologies. It was simply impossible then to imagine the scope of changes that have occurred over the life of these facilities, and it will be increasingly impossible to imagine healthcare needs over the next 50 years or how healthcare will be delivered. Therefore, healthcare facilities must be able to accommodate not only changes we can anticipate but also changes we cannot even imagine.
Design Considerations
The first principle of accommodating change is to design the overall building for layers of change, as out lined by Stewart Brand (1995) in How Buildings Learn: What Happens After They’re Built. The fundamental principle is that buildings designed to accommodate layers of change have long lives. These layers consist of site, structure, skin, circulation, services, space plan and stuff. The key is to design buildings so that more stable elements (“hard spaces”), such as structure and core infrastructure, support frequent changes to the more flexible elements (“soft spaces”) around them.
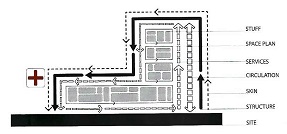
Layers of change. Source: Clemson University Architecture + Health Program
A truly open building system is also designed with a clear hierarchy of circulation where the primary pathways are stable even in the event of changing programmatic use. In cities, we rarely change the location of streets to accommodate the needs of individual development. The most stable elements of the city are its streets and movement systems. Healthcare planners and designers need to employ urban design principles when designing large healthcare facilities and campuses, where movement systems and infrastructure are aligned and stable. Medical planning of a campus, the equivalent of a city block, can then constantly change and transform. Within an open building framework designed for layers of change, modularity can be employed to accommodate flexibility, adaptability, and expandability. Modularity can occur at multiple scales, from building components and individual rooms to planning strategies that allow departments and larger areas to transform. A key aspect of modularity is that it allows for prefabrication. Standardized and prefabricated modules can also lead to improved construction quality in controlling manufacturing conditions, lower waste, and improve the speed of construction. Finally, modularity enables the delivery of high-quality healthcare settings when and where it may be difficult if not impossible to build on-site with locally available materials, expertise and labour. Prefabricated modules are becoming commonly produced at multiple scales:
- Prefabricated and modular casework, headwalls and wall systems
- Prefabricated mechanical, electrical, and plumbing modules
- Prefabricated and modular rooms (toilets, patient rooms, and other spaces that are repeated multiple times in the design and construction of healthcare facilities)
Finally, modularity should be considered in the overall planning of departments and functional areas within them. Standardized clinical modules not only support the implementation of prefabricated building elements but can also help standardize care practices with replicated and pretested design elements.
This note on “The Ability to Accommodate Change” has been adapted from “Chapter 22 – Epilogue: The Future of an Architecture for Health by David Allison, Eva Henrich, and Edzard Schultz” in the book “Architecture and Health: Guiding Principles for Practice Edited by Dina Battisto and Jacob J. Wilhelm” and is fully endorsed by me as relevant and necessary.
Plant-Based Indian Cookbook: Oil, Sugar, Gluten and Dairy Free Vegetarian Recipes
Nandini Gulati and Mala Barua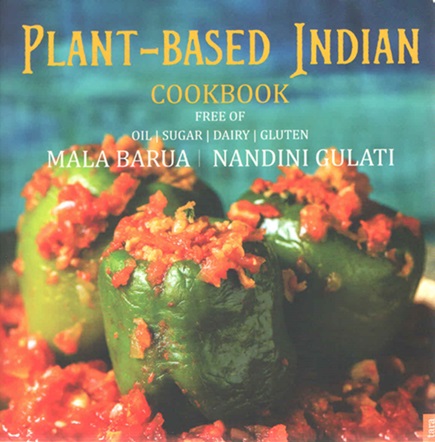 Foreword: Maneka Sanjay Gandhi
Foreword: Maneka Sanjay GandhiFormer Minister, Ministry of Women and Child Development
One of our 33,000 divinities in India is Shakambari, Goddess of Hampi, Karnataka. Every year, on her festival day, she is offered 63 vegetables. They probably have a checklist coming down the centuries because I have yet to find someone who can name that many vegetables offhand. Sadly, we have stopped paying attention to our vegetables and old varieties of grains and seeds. We had over 90,000 varieties of rice in 1960. We now have only 23,000 varieties. Once we had had long red bhindi (okra). No one has seen it for the last 50 years.
I would like to think that India is still largely vegetarian. But the problem is that people mistake drinking milk to be vegetarianism. If the meat of the cow is non-vegetarian, how can the milk from the same animal body be vegetarian? It is for this reason that milk drinkers get the same diseases as meat-eaters – gout, heart disease, cancer, obesity, kidney failure, diabetes…to name a few!
Cows and buffaloes in India, as in most of the world, are riddled with disease. They have been mutated into milk machines and most of them suffer from cancers, leukaemia (Bovine Leukosis Virus or BLV), mastitis, foot and mouth disease, pneumonia, ketosis, brucellosis etc. And are kept alive on antibiotics. I use the word ‘most’ because it is true in over 70-80% cases. All these diseases are zoonotic – which means drinking their milk could make you vulnerable. In fact, scientific studies have repeatedly shown the presence of BLV cells in women’s breast cancer, for instance.
All these animals are given a daily injection of oxytocin, which is a hormone not only to extract the milk faster but which enters the blood and milk stream of the animal. This can cause in humans, everything from early puberty to breast, uterine and prostate cancers, bad eyesight, an imbalance in hair production and more. Milk has been directly related to cancers and diabetes.
The human body is simply not designed to absorb meat or milk. Unlike carnivores, we don’t have canines, claws or slit-eyes with wider vision. Our intestines are too long to eliminate meat easily and our saliva is not acidic. All babies cry when introduced to non-mother’s milk and their burps become smelly. Every child has to be threatened into drinking milk – because the body rejects the idea and it knows best.
Most of these ailments can be reversed through a healthy vegan diet. Doctors in the West have already started a movement in reversing lifestyle diseases through a ‘whole food plant-based’ diet. Ayurveda is a fully researched branch of science that does the same.
Unfortunately, in India people tend to believe allopathic doctors who know very little about diet since the essential science of food and its impact on the human body is not included in the curriculum of medical schools. When a doctor or even a dietician, orders than an ulcer patient should have a glass of cold milk, he will do so not knowing that milk turns to acid in the stomach and will eventually enlarge the ulcer.
Meat eating has become aspirational – just as smoking and drinking beer was in the 1950s. Cooking shows on TV glorify meat and fish dishes. International chefs often scoff at vegetarian food (except if there is cheese or paneer in it) as being boring. However, if you would take a survey of their health issues, most of them will have high blood pressure, high cholesterol, a narrowing of the arteries and almost all of them are overweight.
You don’t have to be vegan to be kind to animals, though taking a moral stand of not causing suffering is extremely laudable. You don’t have to be concerned about the world and its survival even though the methane emitted by animals grown for meat is causing the world to become warmer and the water to dry up. But you have to be kind to yourself. Just as you would not run your stove on petrol, don’t put inappropriate food into your body.
Veganism is not that easy to incorporate into your life. Meat is a drug and once addicted to it, it takes a while to give it up. I would advise that when you are on the road to veganism, stay away from meat-eating environments and people for a while as the smell of cooked meat can bring craving. There will be a few slips along the way but once your body sheds its addiction and goes forward to good health, there is no turning back.
India is a very exciting place to be vegan. There are so many nutritious but forgotten vegetables and grains in India that need to be reintroduced into our daily diet. Black rice from Meghalaya, pineapples from Manipur, 200 varieties of rajma ranging from white to purple, summer and winter millets, thousands of varieties of leaves, berries and fruits that even I need to learn about…
I am as fierce about the organic food movement as I am about animals and nature. I held the first organic festival in India more than 20 years ago. When I became a minister again, I started an annual organic festival in Delhi. Hundreds of women brought produce from all over India. Now these festivals have spread from Delhi to Ahmedabad, Mumbai and Chennai. Customers for organic food have increased every year. I look for women who have regenerated old seeds and old ways of cooking and give them national awards.
I congratulate Maya and Nandini for creating recipes in this book that are easy to cook and are for everyday meals. Vegan and wholesome does not mean exotic or pretentious. It is simply good food with all the bad things kept out – refined and processed ingredients, sugar, oil etc. They have even accommodated the new trend of gluten-free food.
Good food deserves celebration. Good food changes relationships and moods. Good health changes your life and you will never know what it is till you achieve it. This book is a guide. Use it to touch the sky.
From The Authors
Climate Change and Food Choices
Our food has a huge impact on greenhouse gas emissions. Some estimates put it at high as 51% of total emissions. Clearing land for livestock used for meat and dairy is the leading cause of forest degradation. Using pesticides and artificial fertilizers is one of the leading causes of water contamination, degradation of soil quality and loss of bees and insects that are so critical for biodiversity.
Eating seasonal and local food is encouraged as imported food contributes to ‘food miles’ or emissions linked to the distance the food has to travel to get to you.
It is no coincidence that the food that is best for the planet is also best for our health. Locally grown, seasonal, organic and plant-based food has the lowest emissions. Broadly speaking, fruit from native trees requires the lowest input and resources, be it land, water or fertilizers. Fresh seasonal fruit is also easily digestible and bursting with nutrients. Locally grown millets are less resource intensive than the popular rice and wheat varieties. Most local millets require no irrigation and are naturally resistant to pests and insects.
As a thumb rule, if you wish to lower your personal carbon emissions, every meal presents an opportunity to do so. Eat more organic, seasonal, local and fresh plant-based food and you will be cutting out nearly 95% of your food emissions.
Whole Food Plant-Based (WFPB) for Health
Whole food plant-based is more than a ‘diet’ – it is a lifestyle of wholesome eating which shuns all animal-based foods like meat, eggs, dairy, honey and all refined food like oil, sugar, refined white rice and flour etc. It focuses instead on fresh fruits, vegetables, beans, legumes, tubers, seeds, nuts and whole grains.
Additionally, we have gone a step further to curate recipes without wheat to help people looking for gluten-free options. Due to the over-commercialization of wheat, the grains available nowadays are hybrid versions with a high percentage of gluten. Many people are reacting to this high level of gluten showing symptoms of bloating, weight gain, digestive issues and allergies. There are many medical doctors, nutritionists, health coaches and dieticians who recommend this way of eating to prevent and even reverse common lifestyle diseases like diabetes, heart disease, cancer, hormonal issues and auto-immune conditions, among others. To learn more scientific information about this lifestyle, you can see our recommended list of films and books at the end of this note.
How to Make the Change
Switching to a whole food plant-based diet overnight can be a daunting proposition for many, so we recommend a slow and steady approach. Don’t worry if you can’t do everything at once. It’s a skill to be learnt.
We recommend you add a big and juicy salad before every meal. The secret to eating healthy is to eat plenty of fruits and vegetables and as much raw or ‘sun-cooked’ food as possible. In India, we do not give much thought to our salads, lackadaisically cutting up half a cucumber, tomato and some onions as an afterthought to a meal.
The Time Is Now
They say the best time to go for a healthy diet and lifestyle was yesterday and the second-best time is right now!
Today, the same can be said for the health of the planet at large too. Plant-based is the future of food. Thousands across the world are switching their war of eating to more and more plant-based and wholesome food for better health, climate change considerations and most importantly compassion towards animals.
Begin today!
Five Contemplations by Thich Nhat Hanh
This food is the gift of the whole universe: the earth, the sky, numerous living beings and much hard, loving work.
May we eat with mindfulness and gratitude so as to be worthy to receive it.
May we recognize and transform our unwholesome mental formations, especially our greed, and learn to eat with moderation.
May we keep our compassion alive by eating in such a way that we reduce the suffering of living beings, preserve the planet, and be aware of the consequences to our environment.
We accept this food so we may nurture our loved ones, strengthen our community, and nourish ur ideal of serving all living beings.
Resources
In your quest to know more about the vegan and whole food lifestyle, we recommend that you explore the following books, videos and films. They provide the scientific proof and case study evidence of the health, environmental and spiritual benefits of a plant based diet.
Books:
World Peace Diet by Will Tuttle
Eat to Live by Dr Joel Fuhrman, M.D.
How Not to Die by Dr Michael Greger, M.D.
The China Study by T. colin Campbell
WHOLE by T. colin Campbell
Reversing Diabetes by Dr Neal Barnard, M.D.
There is a cure for diabetes by Dr Gabriel Cousens, M.D.
Prevent and Reverse Heart Disease by Dr Caldwell Esselstyn, M.D.
The Starch Solution by Dr John McDougall, M.D.
Milk: A Silent Killer by Dr NK Sharma
Healthy at 100 by John Robbins
Undo it by Dr Dean Ornish M.D. and Anne Ornish
Eat to Live by Dr Joel Fuhrman, M.D.
Disease proof Your Child by Dr John McDougall, M.D.
You can also search for the video lectures by these authors on You Tube
You Tube Videos:
Vegan Video Life Connected
PETA Glass Walls
The Last Heart Attack by CNN’s Dr Sanjay Gupta
Horrors in the Indian Dairy Industry
Films and Documentaries:
Earthlings (www.earthlings.com)
Forks over Knives(www.forksoverknives.com)
Cowspiracy-The Sustainability Secret www.cowspiracy.com
May I Be Frank? www.mayibefrank.com
Eating www.eatingthemovie.com
Vegucated www.getvegucated.com
What the Health (Health)
The Game Changers (Sports and Fitness)
Dominion (Animals)
A Prayer for Compassion (Spirituality)
Most of these films are available on Netflix or YouTube
Levels of Care: Primary, Secondary, Tertiary
There are three classes of primary care practitioners, distinguished by increased sophistication in their level and type of training, as well as by their historical emergence (see figure 3.16) at the lowest level there is a staggering number (roughly 1.1 million) of individual practitioners without any staff (and probably without any qualifications) who are owner-operator of their own clinics; such practitioners are labelled “quacks”. Roughly 80 percent of these are rural establishments located in villages.
One of the reasons healthcare in the USA is so expensive is that doctors have to pay high premiums for malpractice insurance, and this cost gets passed on to the patient. Also, unlike India, there are no “quacks”.
Calvin and Hobbes is my favourite comic strip.
This illustration from Boccaccio’s Decameron shows the Roman emperor Galerius being bled by leeches. According to the text, his symptoms included putrefaction and abominable stench.
A handy medical reference text for physicians was the “leechbook”, perhaps so-called because physicians ere nicknamed “leeches”, from the habit of using these worm-like creatures to drain blood for almost any ailment. Most leechbooks contained remedies of the time gathered indiscriminately from a vast array of sources.
A traditional means to segment delivery across countries is primary, secondary, and tertiary care. These levels have been defined in a variety of ways by a variety of organizations:
Primary care is medical care provided by the clinician of first contact for the patient. Typically, the primary care physician is a general practitioner, family practitioner, primary care internist, or primary care paediatrician. Primary care may also be administered by health professionals other than physicians, notably, specially trained nurses (nurse practitioners) and physicians assistants. Thus, it is the nature of the contact (first compared with referred) that determines the care designation rather than the qualifications of the practitioner.
Secondary care is medical care provided to a patient when referred by one health professional to another with more specialized qualifications or interests. Secondary care is usually provided by a broadly skilled specialist such as a general surgeon, general internist or obstetrician.
Tertiary care is provided on referral of a patient to a subspecialist, such as an orthopaedic surgeon, neurologist, or neonatologist. A tertiary care centre is a medical facility that receives referrals from both primary and secondary care levels and usually offers tests, treatment, and procedures that are not available elsewhere. Most tertiary care centres offer a mixture of primary, secondary, and tertiary care services so that it is the specific level of service rendered rather than the facility that determines the designation of care in a given study.
Primary Care
In terms of overall infrastructure capacity, organized primary care sites comprise an estimated 95 percent or more of India’s delivery capacity, with secondary and tertiary care accounting for 3 and 2 percent, respectively.
There are three classes of primary care practitioners, distinguished by increased sophistication in their level and type of training, as well as by their historical emergence (see figure 3.16) at the lowest level there is a staggering number (roughly 1.1 million) of individual practitioners without any staff (and probably without any qualifications) who are owner-operator of their own clinics; such practitioners are labelled “quacks”. Roughly 80 percent of these are rural establishments located in villages.
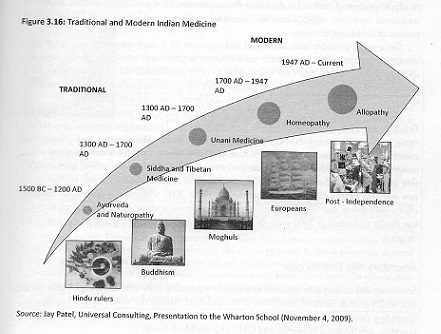
At an intermediate level are practitioners of the Indian systems of medicine (ISM): ayurveda, unani, siddha, naturopathy and yoga. For centuries, they were the traditional suppliers of primary care. During the nineteenth century, these groups were supplemented by practitioners of homeopathy. Collectively they have been referred to as ISM&H, or the more convenient label AYUSH practitioners. These practitioners are typically concentrated in small towns and rural areas. Roughly 75 percent of the populace utilize their services, given their low cost and accessibility. This traditional form of medicine is very popular because the providers consider personal, social, and cultural dimensions of illness and care.
At the highest level are providers of allopathic medicine, which the Indian government began to favour post-independence. The dividing line between AYUSH and allopathic is codified in law and institutionalized in different medical colleges for both. In practice, things are less clear cut, as some practitioners may practice across these boundaries .Neither allopathic medicine nor AYUSH is closely regulated internally or externally, and neither is standardized in terms of qualifications.
Most allopathic physicians are primary care practitioners in solo practice or in small group practices (called “polyclinics”). Three-quarters of them are located in urban areas, providing perhaps a broader range of services than the preceding practitioners, staffed with employed personnel and one or more trained physicians. Roughly one-quarter of the Indian population uses the modern allopathic medicine practitioners who are located primarily in urban areas and who generate nearly 90 percent of healthcare revenues; three-quarters of the population avail themselves of traditional medicine, which is heavily located in rural areas and which accounts for only 10 percent of healthcare revenues.
Secondary and Tertiary Care
Secondary and tertiary care rendered in hospitals was traditionally offered through public facilities which provide services free of cosy or at subsidized rates to the lower-income populations. Secondary facilities are found at different administrative levels in each state, including district hospitals, sub-divisional hospitals, and CHCs (at the block level).
Since the mid-1070s (and especially after the 1991 market liberalization), the Indian government has provided a host of incentives to expand facilities in the private sector, including land concessions, tax breaks, low-income loans from public banks, transfer of public hospitals to private firms, duty exemptions for imports of medical equipment, rebates in customs tariffs, reimbursement for government employees, and allowances for hospitals to be run as tax-exempt “trusts.”
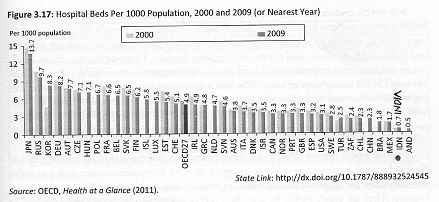
Not surprisingly, statistics on India’s bed capacity also vary widely. The count seems to depend on whether or not nursing homes are included. Across all facilities, there are 1.2 million to 1.7million beds, if one considers only hospitals with 30 or more beds, the count is 680,000 private hospital beds. Despite the large number of hospitals and beds, world benchmarks suggest that India suffers from a lack of capacity (see Figure 3.17). Compared to OECD and select other nations, India ranks second to last with 0.7 beds per 1000 population (versus the OECD average of 4.9). India ranks unfavourably when compared with the world average of 2.6 beds as well as the capacity found in other emerging markets (2.3 beds in China and 1.8 beds in Brazil).
As in the US, bed statistics can be decomposed into licensed beds and staffed beds; the former represents potential capacity, while the latter reflects what the hospital can actually staff and utilize for patient treatment. Data from TechoPak suggest that 30 percent of private beds and 50 percent of public beds are “non-functional” due to lack of personnel. Using their base of 1.37 million beds, there are 853,000 operable beds in the country (consistent with the OECD bed/population ratio).
Overall, in spite of a majority of the population residing is rural areas, the distribution of hospital bed capacity is noticeably skewed in favour of urban India, where roughly three-quarters of both public- and private-sector beds are located. Nonetheless, even for many in close proximity to urban hospital facilities, “socioeconomic distance” has proven a barrier to healthcare access: basic measures of health for the poorest 40 percent of the urban population remain at par with the substandard levels observed in rural areas.
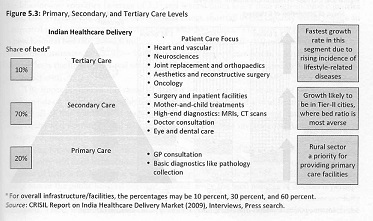
The above extract, Levels of Care, has been adapted from the book ‘India’s Healthcare Industry: Innovation in Delivery, Financing, and Manufacturing – Chapter 2 – An Overview of the Value Chain’, edited by Lawton Robert Burns. This book has been published in 2014, so the statistics are dated accordingly. It is presented here to put the efforts of Indian healthcare architects in context.
On Strategy for Healthcare: Will Disruptive Innovations Cure Healthcare
A Bit of Context
This article made the competitive threats and opportunities in health care explicit when it was published in 2000. Its messages are now even more compelling, as competition on value rather than brand is increasingly driving the health care marketplace, and as a wired world enhances the feasibility of meeting patients needs in so many new, more convenient, and less expensive ways. If in-office care is a potential disruptor, as portrayed in this articles well-known graph, “Disruptions of Health Care Institutions,” the race is on to develop models that make the office visit a secondary or even more later option in meeting patients’ needs.
The authors’ “disruptive innovation” framework also helps explain why health care leaders must recognize that fighting against the outward trend of health care services is a losing battle, as they shift from the high-cost centers where many were invented, towards lower-cost and more convenient sites of care. The natural sequence goes like this: An academic medical center where expert clinicians and researchers work shoulder to shoulder develops a new test or procedure. Its value is proven in research studies. At first, patients flock to the one or several medical centers that offer it, but once the bugs are worked out, other well-trained clinicians can perform it. Soon, community hospitals offer the test or procedure. Then doctors’ offices. And then, in some cases, other settings, including patients homes
If you are a leader in an academic medical center or any of the other stopping places along this path-but only one stopping place-you naturally don’t want the expertise to migrate outward. You want the patients (and the revenue) to stay with your organization. So you resist, using tactics such as pushing for regulations that make it difficult for the test or procedure to be performed in other settings. In doing so, you are setting yourself up to be a casualty of the disruptive innovation that will inevitably rise-somewhere else.
Instead, recognizing these dynamics at work, many health care organizations are merging vertically, that is, acquiring the downstream lower-cost sites to which they would otherwise inevitably lose business. Moving to own more of the options is a step in the right direction, as it at least reduces the reflexive resistance to movement outward. But, to compete successfully and thrive in today’s marketplaces, more is needed than these opportunistic mergers. Health care leaders should ask how disruptive innovation represents a threat they are at risk for ignoring and an opportunity they should seize as they compete to improve the value of care.
-Thomas H. Lee
—————————————————————————————————————————————
Idea in Practice
Disruptive innovations in other industries offer lessons for transforming health care:
• Create a system that matches clinicians’ skill levels to the level of medical difficulty.
Use technology to channel simple problems (e.g., strep throat) to clinicians who can follow predictable rules for diagnosis and treatment. For example, expand nurse practitioners’ role as primary care providers and provide tools that allow them to accurately refer more complicated conditions to more sophisticated diagnostic abilities.
• Invest more money in technologies that simplify complex problems, and less in high-end technologies.
Today most R&D dollars go to complex solutions for complex problems. But more venture capital must flow to projects focused on technologies that simplify diagnosis and treatment-especially of common diseases. By launching a series of such disruptive business ventures, major health care companies (Johnson & Johnson, Baxter, Merck) could spur significant growth – with less investment. c • Don’t be afraid to invent the institution that could put you out of business.
We’ll always need some general hospitals for critical care (just as we still need mainframe computers after PCs transformed that industry). But most health care needs can be better met through specialized institutions that provide state-of-the-art care for a single category of disorders, such as cardiac or renal illness.
• Overcome the inertia of regulation.
Instead of working to preserve the existing system at all costs, regulators should be asking “How can we enable disruptive innovations to emerge?” Example: An entrepreneur creates a portable X-ray machine for use in medical offices rather than in hospitals – promising significant cost savings. Regulators could support the new technology and address any concerns about possible risks. How? Require that all images interpreted by non-radiologists be transmitted via internet to a second-opinion center. There, skilled radiologists could check or confirm initial diagnoses.
The progress of disruptive innovation
Dominant players in most markets focus on sustaining innovations – on improving their products and services to meet the needs of the profitable high-end customers. Soon, those improvements overshoot the needs of the vast majority of customers. That makes a market ripe for upstart companies seeking to introduce disruptive innovations – cheaper, simpler, more convenient products or services aimed at the lower end of the market. Over time, those products improve to meet the needs of most of the market, a phenomenon that has caused many of history’s best companies to plunge into crisis.
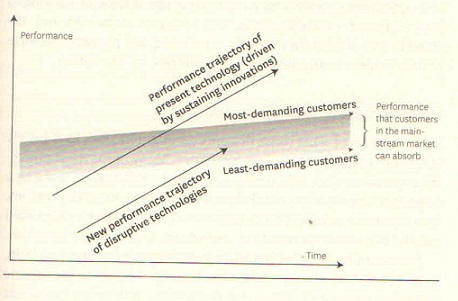
Disruptions of health professions
As specialist physicians continue to concentrate on curing the most incurable of illnesses for the sickest of patients, less skilled practitioners could take on more complex roles than they are currently being allowed to. Already, a host of over-the-counter drugs allow patients to administer care that used to require a doctor’s prescription. Nurse practitioners are capable of treating many ailments that used to require a physician’s care. And new procedures like angioplasty are allowing cardiologists to treat patients that in the past would have needed the services of open-heart surgeons.
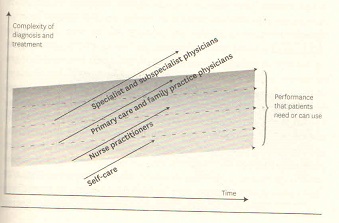
Disruptions of health care institutions
Teaching hospitals incur great costs to develop the ability to treat difficult, intractable illnesses at the high end. In the process, they have come to over-serve the needs of the much larger population of patients whose disorders are becoming more and more routine. Most types of patients that occupied hospital beds 20 years ago are now being treated in more-focused care centers and outpatient clinics, doctors’ offices, and even at home.
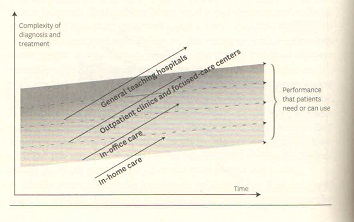
The above extract is from the book “HBR’s 10 Must Reads – On Strategy for Healthcare” from the article “ Will Disruptive Innovations Cure Health Care” byM. Christensen, Richard Bohmer and John Kenagyand is presented here for my Healthcare Management readers. This very good book is available on Amazon.in at a reasonable price.
Future Healthcare Design: The Five Constants of Healthcare
In The Context of the National Health Service (NHS), UK. The importance of healthcare has long been understood and valued; however, the importance of healthcare design is not well understood and doesn’t appear to be valued. Whenever I visited hospitals – private, state-run and charitable – I became curious of healthcare design. Common patterns began to emerge – and inspiring solutions, too. While other areas of public architecture such as schools, libraries and housing have had a continuous history of design development, and even aesthetics, hospitals have suffered from a stop-start timeline despite advances in technology and medical care. Five themes recurred during my research for this book, not only in the UK but also globally. These are what I have called the five constants:
- Attachment
- Money
- Risks
- Silos
- Reorganization
Attachment
There are many forms of healthcare buildings, including GP Surgeries and community healthcare buildings, but it is the hospital building to which we feel most viscerally connected. And for a good reason, too. It is the place where all our insecurities about our biological and psychological lives are played out; it is the theatre where we witness the drama of our own mortality from birth to death; it is where we place our lives and those of our loved ones in the hands of strangers we trust to make everything all right again. It is no wonder that hospitals have provided so much entertainment in the form of films, TV dramas and documentaries. Our attachment to hospitals is also the reason why people donate generously to the cost of their building. This attachment provides a strong engagement with healthcare buildings – a connection that can be useful for creating patient-centered designs using participatory design methodologies. Durability and functionality are two of the three qualities of architecture specified by the Roman architect and engineer Vitruvius (the third is beauty). Henrik Fisker, the car designer who conceived the Aston Martin DB9, said, ‘I believe good design is about finding beauty – an emotional connection with the consumer..’ Attachment through beauty is a strong human emotion, and it can be used to create better designs and a sense of ownership over the building.
Money
Money is the lifeblood of hospitals and it is very limited and precious, even in wealthy countries. When healthcare staff refer to efficiency and sustainability, it is always in the context of money. The NHS suffers from chronic lack of investment in its services and estates. The most recent NHS funding increase of January 2019 remains below the average increases of 3.7 per cent a year since the NHS was founded and is less than the 4 per cent annual increases that are necessary to meet rising demand and maintain standards of care. However, it is worth noting here that despite the calls for greater efficiency, the NHS is actually 10 times more efficient than the UK’s economy. During 2016-17, the NHS delivered 60 per cent more ‘care’ per year than in 2004, including 5.2 million more operations a year and 60 million more patient appointments. Despite not getting funding increases for staff, medicine and repairs, pound for pound the NHS delivered 16.5 per cent more care in 2016/2017 than it did in 2004/2005, while the wider economy grew by just 6.7 per cent. In London’s most dilapidated hospital, ice cream distribution continues in hot weather because the windows don’t open, while beds have to be pushed away from the walls during rain, and an ambulance is used to move patients in parts of the estate to find a lift than works. Ironically, even this hospital delivered London’s best A&E performance in 2017.
Risks
Around the world, most hospitals of all kinds have boards with non-executive directors from the private sector, working alongside the executive directors. While the CEO’s and executive team are people who have worked their way up or may have studied management (apart from the medical and nursing directors), the non-executives come from many different background such as medicine or nursing, social care, the charity sector, banking, surveying and law. The intention is that the private sector brings ideas and challenges to the executive team. In practice, this doesn’t always work because healthcare delivery is risky and money is limited, while healthcare delivery is highly regulated. In particular, medical mistakes are very expensive. The 2017/2018 NHS balance sheet for medical negligence was estimated at UK pounds 77 billion out of its UK pounds 122 billion overall budget. Mistakes also come with reputational risks, and one can understand why NHS boards might be generally risk averse. This means that in the delivery of healthcare buildings, risk taking in the form of new designs which could influence ways of working may not be welcomed. While most staff might want a better working environment, they also dislike the disruption that construction work invariably brings. However, there are risks to working in buildings that do not support today’s IT systems or comply with fire regulations. In procuring healthcare designs, risks are reduced by having various mechanisms via which unfamiliarity is reduced. There’s a tendency to rely on ‘frameworks’ that weed out potentially risky suppliers, including architects. Smaller or internal projects make use of the in-house estates teams for ‘design’ instead of architects. Other ‘safe’ relationships include choosing a company or a person who have been worked with before. However, better managed healthcare trusts take more risks and are more likely to consider innovation. Mistakes can be still made (as can be seen from the long list of NHS enquiries and reports; e.g. the Francis report), but failure can be a positive thing because improvements also come out of a rigorous examination of failures. In 2018, the Good Governance Institute organised a round table about the differences in the appointments of artistic and medical directors. For arts organisations, the artistic director leads the strategy, balancing risk appetite while pushing the brand image, for the medical director (and other executive staff), strategy is driven by finances, risk avoidance and regulatory compliance. Thus, the end results are very different.- one is expansive and the other is restrictive.
Silos
Effective design solutions require collaboration between healthcare team members – but there are often information silos in hospitals, nursing data is not shared effectively between departments. Architects are used to working in teams and therefore they might find the healthcare working environment very strange. Furthermore, many capital developments are estates led rather than strategy- or service-led, leading to operational problems. Existing pressures on facilities and opportunistic approaches can lead to poor decision-making on long term capital projects and strategic planning. Presently, the NHS estate is scattered across 250 trusts and foundation trusts, NHS Property Services and Community Health Partnerships, which are located within hundreds of areas called Sustainable Transformation Plans (STPs) and Integrated Care Systems (ICSs). However, the organisational set-up of hospitals can also impede the deign process. In the past, trusts were encouraged to compete both internally and externally and this mentality continues. In one trust based in London, such competition led to death, and a 2018 enquiry found that internal scrutiny of the department was ‘inadequate’ and the surgeons were split into two camps exhibiting ‘tribal-like activity’. But this is not new. In 1930 Gordon Friesen, the Canadian hospital planner, said ‘most hospitals today are made up of little kingdoms, all ruled by influential staff members. Now, if you ask each of these people what they need, they will ask for things which perpetuate their kingdoms.’ Design engagement with different teams within the healthcare provider can become difficult due to this attitude.
Reorganisation
Healthcare, particularly as delivered by the NHS, has been restructuring almost since it was formed due to increasing demand and decreasing money. Reorganising is perceived as progress, as in this satirical observation: ‘every time we were beginning to form up into teams, we would be reorganised. I was to learn later in life that we tend to meet any new situation by reorganising; and a wonderful method it can be for creating the illusion of progress while producing confusion, inefficiency, and demoralisation.’ Even more capricious have been hospital management systems which affect healthcare estates. The NHS leases estates from local authorities, private companies and PFI providers, while thousands of individual GP Practices own their own premises. Such disparate elements affect the NHS’s strategic capability for capital planning. The pace of policy change far outstrips capital development plans, while timescales for strategic plans and capital developments are rarely aligned. There are very few individual organisations that have appropriately trained board-level estate leads (let alone architects or planners) to be able to engage effectively across the system. Though this constantly changing landscape is difficult to navigate, it may also help to open up areas for future work in healthcare design.
What can architects do for future healthcare design?
Healthcare design presents a strange conundrum. While medical technology and delivery have become smaller, faster and more portable, they are used inside cumbersome buildings that are difficult to adapt and use. But this is exactly why the architects role in healthcare will continue to evolve and become increasingly important, as hospitals seek to find value for money with ever-diminishing capital budgets.
The value of design may not be something that is understood by the staff, who are used to working in the most challenging circumstances. Although admitting that users are heavily influenced by the environment in which they work, a British doctor justifies this situation: ‘We know that fellow professionals can and are achieving wonders in helping patients in the most primitive accommodation and circumstances around the world. I suggest we should not only be grateful that most of us are not trying to practise under conditions of open warfare, flood, fire and famine, but should make the very most of our (for the most part) privileged clinical and professional environments.’ But as the NHS is the largest single employer within the EU, employing 1.5 million people, it is morally unacceptable to make them work in poor environments. Plus, as we will read later, this also makes for poor patient experience and endangers patient safety.
According to a survey of medical professionals in the US in 2014, 85 per cent of them did not receive any information about the impact of buildings upon health, even though they knew that the buildings have an effect on the occupants. The authors of the report concluded simply that architects and designers should continue to connect with clinicians. The NHS used to have a Chief Architect, but the role played by architects in the public sector has diminished. Though in 2019 the Ministry of Housing Communities and Local Government has created a new post of ‘Head of Architecture’, knowledge about architectural services is very poor. In a survey conducted by YouGov in 2012, 15 per cent of Britain’s population did not know what an architect does. Twenty-two per cent did not know that architects prepared detailed construction drawings for building projects, 48 per cent did not know that they prepare building specifications, while 72 per cent didn’t know they applied for planning permission.
Design is not a subject taught in school in the UK. In life, price is usually valued over design, a mindset ingrained daily through habit. Quantity is valued is valued and understood more than quality. This might explain why more accountants and quantity surveyors sit on the boards of NHS trusts, than architects, designers, artists or psychologists.
The general assumption is that design means how something looks – as an NHS executive put it to me, ‘I care about functionality, I don’t care about design.’ Steve Jobs explained the paradox: ‘Design is a funny word. Some people think design means how it looks. But of course, if you dig deeper, it’s really about how it works.’ Within healthcare, beauty is viewed as a frivolous matter – an unnecessary, expensive thing.
If saving money is a big concern, then an increasingly relevant area where architects can contribute is the design of sustainable buildings for healthcare. Hospitals are very energy-intensive buildings, and need air-conditioning, lifts, water purification, incineration of bio-hazards and other services. If healthcare were a country, US healthcare would be the world’s tenth-largest carbon dioxide emitter. Goals can be set towards the best possible energy rating (LEED or BREEAM), whether the building is new, an extension or a retrofit. This is not just for economic reasons but also for the wider social responsibilities of a healthcare building.
Sustainability is embedded in the NHS constitution with an emphasis on ‘the most effective, fair and sustainable use of finite resources’, yet it is responsible for 18 per cent of carbon dioxide emissions of non-domestic buildings in the UK – 30 per cent of all public sector emissions. Twenty-two per cent of these come from building use, 18 per cent from travel and 59 per cent from procurement. It is perfectly possible to cut these emissions particularly those relating to energy-intensive procurement, by sources products and services that are climate friendly and ethical. In fact, the NHS supply chain provides a code of conduct for this, but it doesn’t seem to be used effectively because cost savings are prioritised. However, energy costs are expected to increase at a rate above inflation, demanding an increasing share of NHS budgets. It has been estimated that energy-efficiency measures could cut this bill by up to 20 per cent, saving the NHS UK pounds 150 million each year. So, saving the planet can also save money.
However, this requires capital investment of up to UK pounds 1.5 billion (based on a 10-year payback) – this may significantly add to the existing backlog maintenance. The Department of Health provided only UK pounds 49.3 million in 2015 for over 100 energy efficient projects to 48 NHS organisations in England, so this is a significant shortfall that needs to be made up over the coming years. But it is also possible that a well-designed passive building might not need solar panels or other gadgets.
Clean water is one of the scarcest resources on the planet but vital to modern healthcare, so efficient use of water could yield significant savings for the NHS. An exemplary water-saving programme at Guy’s and St Thomas’ has reduced the trust’s water consumption by nearly 20 per cent, and this saving of UK pounds 120,000 went to the charity WaterAid to provide safe water and sanitation in Nepal. Great Ormond Street hospital has also introduced rainwater and grey water recycling.
As the theory of culture lag suggests, alteration of values is likely to be slow and evolutionary, while changes in material culture are quick and revolutionary. This may explain why the NHS in particular is quick to embrace technological changes (material) but not design advances (value). The challenge for architects is to convince healthcare providers that good design involves the delivery of all the things on their ‘worry list’ – that design is a way of improving health. The authors of a paper titled ‘Architects, Urban Design, Health and the Built Environment’ propose that there are three types of architects: architects (who) desire to be the star of the moment (fashionistas), those who focus on the improvements of functions for humans (life improvers), and those who focus on creating packages that include both a design and the services that accompany it (object-service packagers). They say that the future of healthcare architecture lies in the third role of object-service packagers, i.e. those who focus on bundling objects and services related to improving health. This collective approach should be the goal for governments, clinicians, patients and architects all over the world.
Design as way of solving healthcare problems
The focus of the healthcare facility should be on the patient first, and processes should follow. The human body as a ‘machine’ was described by Descartes in his book Treatise on Man (1662), while Le Corbusier called the house a ‘machine for living in’. In the same vein, hospitals can appear to be like factories. Design processes used by the car industry are often replicated in the NHS to show efficiency and cost savings, but patients are not cars. Furthermore, a healthcare facility is not a sealed environment like a car factory. How can the design process of healthcare buildings become more humanised?
A design tool from the Design Council is the ‘Double Diamond’. Four stages are organised to create a system of designing. The expansive phases of the Diamond represent the divergent thinking that embraces many issues, while the pinch points represent the coming together of those ideas and thinking – the convergence. The Double Diamond indicates that this happens twice – once to define the problem, and then to define the solution. However, this approach imagines the architect being a team leader, like in a traditional contract. Today, most healthcare buildings are procured by D&B, or via a Framework, so this has been adapted to current healthcare procurement.
- Understand: Understand the specific concerns of the healthcare provider, be it specialist, acute, general or community care. Remember, what underpins good healthcare design is good patient experience.
-
Uncover: This would be the initial survey of design requirements for the healthcare facility. This stage is about revealing the fundamental blocks to making the desing patient-centered and thinking outside the regulatory box.
- Unite: This is the inch point, where understanding the concerns leads to the formation of a ‘vision’, literally the coming together of the understanding of the project and an aspiration in as simple words as possible, such as ‘A hospital that doesn’t feel like a hospital’. A good vision will unite all users – staff, patients and visitors.
- Uplift: The role of the architect in a healthcare environment is to provide an uplifting design based on a creative vision for the facility. This may be challenging due to the past constraints and habits, particularly the tendency towards risk avoidance and therefore going for what is safe.
- Use: The intelligence and evidence gathered so far should provide the design solutions that unite and uplift all users.
In a survey in 2011, Patient Opinion analysed the 537 most critical responses of the 2,537 negative comments it received. The top complaints were about staff attitude and waiting times, regardless of the type of hospital. Can architects help to find design solutions for these two problems? Hospital staff must provide both medical and psychological support patients, sometimes in traumatic situations. Staff working night shifts suffer from sleep deprivation and stress. In addition, many staff suffer from musculoskeletal disorders as a result of lifting and stretching, and from hospital infections. Woking in such conditions can affect staff attitude.
The above extract is from the book “Future Healthcare Design” from the chapters “Introduction” and “The Brief and the Process” by Sumita Singha and is presented here for my Healthcare Architect readers. This very good book is available on Amazon.in at a reasonable price.
For Health, You Needn’t Have Wealth
By Dr Devi Shetty
Here’s how govt can ensure very affordable health insurance, including for outpatient care, for hundreds of millions of Indians who are neither poor nor rich
Countries that have managed ‘universal healthcare for free’ through taxation have three things in common. They are invariably small countries with a high tax-to-GDP ratio of more than 30% and spend more than 10% of their GDP On healthcare.
India is the world’s most populous country with a tax-to-GDP ration of 11.7% and spends 3.16% of the GDP on healthcare. The government’s contribution is 1.28% and out-of-pocket health expenditure is 1.52% of GDP. We can’t expect the government to enhance budgetary allocation to healthcare significantly.
Fortunately, the Ayushman Bharat scheme covers the population living below the poverty line. But what about the millions of Indians who are one medical bill away from slipping into poverty?
Although 300 million middle-class Indians cannot afford to pay for the hospitalisation, they can pay for affordable health insurance. So, our national narrative should change from ‘universal healthcare’ to ‘universal health insurance’-which should cover primary, secondary and tertiary care through integrated health insurance.
 In the integrated health insurance model, hospitals will become the health insurance providers and work hard to ensure that members don’t fall sick to save money, thereby aligning the interest of the patients and the hospitals. This will also address the patient’s fear of unnecessary procedures.
In the integrated health insurance model, hospitals will become the health insurance providers and work hard to ensure that members don’t fall sick to save money, thereby aligning the interest of the patients and the hospitals. This will also address the patient’s fear of unnecessary procedures.Why change from current health insurance which pays for hospitalisation to integrated health insurance?
About 14% of the heart surgeries performed in India are done by our group of hospitals-the more people develop heart attacks the better it is for our business. There is absolutely no incentive for us to keep people healthy. In reality, in any business, if the interest of the customer and the service provider is not aligned, there is no trust.
In the integrated health insurance model, hospitals will become the health insurance providers and work hard to ensure that members don’t fall sick to save money, thereby aligning the interest of the patients and the hospitals. This will also address the patient’s fear of unnecessary procedures.
Why is primary care very important?
About 30% of Indians visit primary care physicians at least twice a year. Over 60% of healthcare expenses are due to outpatient care which most health insurances do not cover. Uncontrolled diabetes and blood pressure which lead to heart attacks, brain strokes, and kidney failures can easily be controlled by hospitals online. With early detection, most diseases can be cured.
What is the ideal integrated health insurance model?
By trial and error, the aim should be to achieve an integrated health insurance model with an annual premium at about Rs 8,000-10,000 for a family of parents and all the children less than 21 years. Parents should undergo health check-ups costing about Rs 15,000 by paying a token amount of Rs 1,000. Health screening is very important for early detection.
Apart from unlimited outpatient coverage families should be covered for multiple admissions up to Rs 10 lakh and single admission up to Rs 50 lakh, to cover complex procedures like transplants and artificial hearts.
Health insurance experts will certainly disagree with the amount of premium. That was our experience 17 years ago when we conceptualised “Yeshashwini’ micro insurance in the state of Karnataka. We believed that if every farmer in Karnataka paid Rs 5 per month, they could be covered for any surgery from cataracts to heart surgeries at over 700 hospitals. The state government launched the scheme through cooperative societies and became a reinuser and then the magic happened. At the end of 12 years 1.21 million farmers had surgeries and 1.3 lakh farmers had cardiac procedures just by paying Rs 5/month.
How do we make health insurance premiums affordable to the middle class?
‘Health Savings Account’ is a platform for people to save money to pay for healthcare which is implemented successfully in many countries.
- In India with over 90% of the workers employed by the unorganised sector, HAS can be implemented by converting ABHA (Ayushman Bharat Health account) into a wallet funded via UPI, so HAS and electronic medical records can be captured digitally in one place.
- The unorganised employer should contribute Rs 100/month or more to the employers HAS account.
- Employer, employee or donors’ contribution should be exempted from taxes and the money used only for buying health insurance.
- A few thousand rupees of contribution to HAS will offer few lakhs of benefits to the deserving family.
- This will be the first step in shifting unorganised workers to the organised sector.
- If 18% GST on low-cost health insurance premiums is exempted, then the health insurance providers can arrange interest-free loans for the premiums through NBFCs.
For social upliftment we believe the government should utilise the power of creating a regulatory framework for the private sector to innovate, take risks and deliver rather than spending the money directly. If 100 million middle-class families contribute Rs 10,000 per year as the health insurance premium, Rs 1 lakh crore can be raised which is more than the health budget of the government.
In a short period of time, we have grown from radios to colour TVs with a few hundred channels, from no phones to smart phones, and emerged as the world’s largest online payment provider. With an affordable digital health insurance platform, we can become the first country in the world to disassociate health from wealth in just five years and prove to the world that the wealth of the citizens has nothing to do with quality of healthcare they can enjoy. This is the power of India with 1.4 billion people managed by the government with a vision and belief in technology.
This article taken from the newspaper The Times of India, Monday, January 30, 2023.
The writer is a cardiac surgeon and Chairman and Founder, Narayana Health.
Sustainable Design: Ecodesign: What and Why
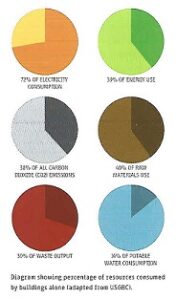 As designers we have a divided set of responsibilities. Professionally and contractually, our primary obligation is to our clients, including a mandate to protect public safety. Artistically and financially, we also have certain obligations to ourselves. Beyond these, though, we have a duty to the public in a larger sense than the safety issues that licensing addresses. That ethical responsibility, which considers how our built designs affect the world, is both professional and personal.
As designers we have a divided set of responsibilities. Professionally and contractually, our primary obligation is to our clients, including a mandate to protect public safety. Artistically and financially, we also have certain obligations to ourselves. Beyond these, though, we have a duty to the public in a larger sense than the safety issues that licensing addresses. That ethical responsibility, which considers how our built designs affect the world, is both professional and personal.One way to view this is to interpret public safety as encompassing environmental issues, for without the support of the Earth’s ecosystems, human life would be threatened. We could not survive without the air, water, and atmospheric protection that our exquisitely tuned planet provides. Our lifestyles, if not our lives, are reliant on the “free” ecological services – oxygen creation, water filtration, nitrogen fixation, etc. – that we too often take for granted. It is by no means a leap, then, to say that a primary
Its become a truism that green design is a valuable and necessary goal. But it’s worth taking a few moments to establish just how important it is, before getting to what it is. Buildings are not only the cause of ecological issues. Blame can be shared with population growth, transportation, industrial agriculture, carnivorous diets, and our sometimes irrational desire for ever more stuff. How important are buildings in this gathering storm?
In 2003, Edward Mazria, who was a green architect before such a category existed, looked closely at the statistics of energy consumption in the United States and concluded that the role of buildings was far greater than expected, amounting to 48 percent of U.S. energy consumption and 46 percent of U.S. carbon dioxide production. These statistics convey a significant point: climate change and other environmental issues are not somebody else’s problem: they are ours. They are not issues to be passed off to the worlds of governrnent, though they, too, bear a large part of the responsibility. Buildings are put creation, and with that comes the need not only to make them durable, functional and good-looking but also to ensure that they are good citizens.
Marzia’s numbers were eye-opening for the architecture and design community, sparking renewed concern over the role of buildings in our energy usage and dependence. Shortly thereafter, the film An Inconvenient Truth drew further attention to these issues. In the process, though, other no-less-than- important – such as water pollution and usage, resource consumption, the effects of toxic materials, and social and ethical dilemmas – have sometimes been de-emphasized. While energy conservation and alternative energy development are indeed critical, a more holistic approach to design and construction is needed. The more encompassing objective is to ensure the well-being of our communities and the ecosystems that surround them for current and future generations.
And when we adopt this broader vision, we can begin looking anew at additional questions, asking what the role of a building should be. We tend to view buildings as discrete, individual objects inserted on the planet. A holistic view would see them as systems both unto themselves and inseparably tied to surrounding ecosystems.
Redefining the role of buildings and our relationships to them can take us in new directions artistically (what does an ecobuilding look like?) and beyond if we are modifying the goals of design to change what it is designers do.
The Beginnings of Green Design
What do we actually mean when we talk about green design, sustainable design, or ecodesign? Generally speaking, we can apply these terms interchangeably. While there may be nuanced differences between them, I find it more helpful to think in terms of what we are trying to achieve.
Ecodesign has evolved considerably from its 1960s origins, captured in the phrase “reduce, reuse, recycle.” The catchiness of the now ubiquitous three Rs helped immensely in expanding awareness, but that same simple edict has led some people to conclude that once they’ve recycled their bottles and newspapers and converted a light bulb or two, they’ve done their part.
Similarly, designers who have included three R-type type thinking, which can be thought of as the first level of ecodesign, may feel that their jobs are done. These are the tweaks described earlier, incremental changes that, while positive in general, do not go far enough because their goals are too limited or because they look at issues in isolation instead of holistically.
Cradle to Grave
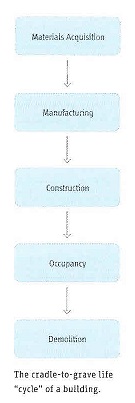
To get beyond this crucial but narrow starting point, the concept of ecodesign has to be broadened. The first step in achieving this is to look at what is called, somewhat inaccurately, the life cycle of building and materials. Life cycle analysis (LCA), also known as life cycle assessment, has been applied more frequently to products, but the principles also apply to buildings. The life of the product (or building) is examined from cradle to grave; that is, from the origin of its raw materials to the manipulation of these materials during manufacturing, to the consumption of energy and resources during its useful life, to the impact of its eventual end of life.
At each phase of the life cycle, there are material and energy inputs and corresponding environmental impacts. An LCA attempts to quantify all of these inputs and then come up with values to represent their impact. By analyzing the results of an LCA, a designer can evaluate where to improve or modify a creation; is it, for instance, more beneficial to increase energy efficiency, replace toxic materials, or convert to recycled materials?
The cradle-to-grave approach, while more encompassing than the three Rs, still has limitations. The use of the word grave implies that buildings and products have a linear life span. In this sense, life cycle analysis is a bit of a misnomer. Another shortcoming, in the words of ecodesign advocates Bill McDonough and Michael Braungart, is that the cradle-to-grave approach amounts to merely “being less bad.” It enables us to see and reduce the overall impact of what we build, but it does not get us to the goal of sustainability.
Cradle to Cradle
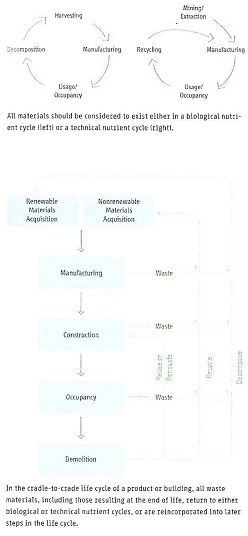
Putting the cycle back into life cycle analysis is the next conceptual leap we must make. This represents an expansion from cradle-to-grave to cradle-to-cradle thinking. Though this idea was popularized by McDonough and Braungart in their book Cradle to Cradle: Remaking the Way We Make Things, it has deeper roots, perhaps originating with Buckminster Fuller’s Operating Manual for Spaceship Earth, in which Fuller compares the Earth to a spaceship starting its journey with a finite amount of resources that cannot be resupplied. This concept was driven home in 1968 by the iconic image from Apollo 8 of our planet isolated in space. With that photograph in mind, pondering how we make things and where the materials come from will quickly lead to a visceral grasp of Fuller’s prescient point. Our materials (iron, coal, oil, agricultural nutrients, etc.) as well as the air and water we require for life, do not get replenished from outside the Earth’s closed system floating through the universe, Everything we have and ever will have is, in one form or another, on the planet now. (Given the tremendous cost and energy of spaceflight, we are unlikely ever to bring back useful quantities of materials from other planets.) Therefore, to be truly sustainable, we must never use up resources faster than the Earth’s ecosystems can replenish them.
However, there is one critical exception. Because solar energy is constantly replenished, falling on the Earth every day, we can use it without fear of running out. This includes energy derived directly from sunlight, as well as related renewable sources, such as wind and biofuels, that would not exist without the presence of the sun and, by loose extension, tidal and geothermal energies.
Prior to humanities presence, the Earth existed with the fundamental constraints for eons and therefore developed ingenious systems in which nothing is ever discarded. If it had not, some resources would have been exhausted over time. But nature is an expert at efficiency and symbiosis and long ago demonstrated a concept that we verbalized only recently: waste = food. This doesn’t refer literally to food that we throw out, but to all kinds of waste – organic, inorganic, industrial, residential – and signifies that everything we think of as garbage must become an input for another use. Landfills, by this measure, are wasted resources, a sign of gross inefficiency, and they represent a failure to follow the instructions in Fuller’s Operating Manual.
McDonough and Braumgart divide everything we might consider waste into two primary categories: biological nutrients and technical nutrients. Biological nutrients are materials that, after we are done with them, can be safely returned to the earth and therefore need to be kept in cycles of usage – they need to be recycled. Petroleum-based plastics are a good example.
There are also materials that are both unrecyclable and unsafe to put back into ecosystems (e.g., nuclear waste and toxic chemicals). Because these are so expensive to deal with and because they have no place in a cradle-to-cradle system, these are to be avoided at all costs. Composites of materials that cannot be separated after use and so cannot become either biological or technical nutrients are also problematic. McDonough and Braumgart call these “monstrous hybrids.”
The Triple Bottom Line
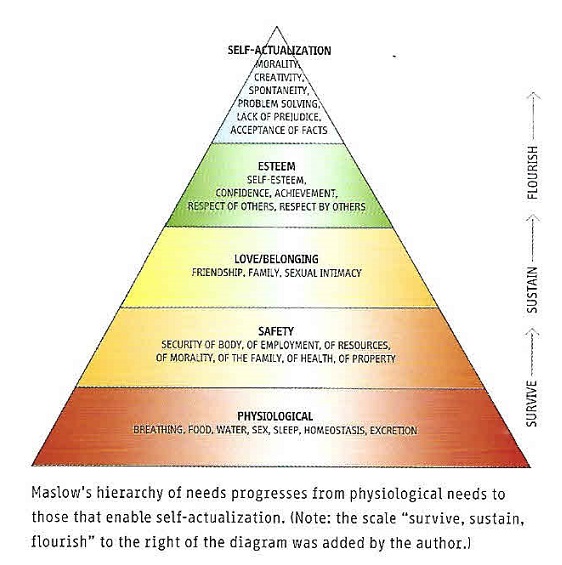
So far, we’ve been looking at green design in terms of environmental impacts. True sustainability, though, requires us to broaden our definitions to include aspects of how we live. How are the people who make things treated? How are their communities affected? How are the economic and social inequities among regions of the world dealt with? How do our buildings affect their occupants and local communities? This can be thought of as the fourth level of ecodesign, building upon the ecological foundations of the three Rs and the cradle-to-grave and cradle-to-cradle approaches.
In conventional business practice, the standard gauge of success is the bottom line: is the company making money? In the world of green business, an alternative gauge has evolved. The triple bottom line concept adds two criteria alongside the financial one: how the planet is treated and how people are treated. The three bottom lines are frequently referred to as “people, planet, and profit” or “ecology, economy and equity.”
Putting numbers to ecology and equity is a very complicated and controversial process, but the concept that good business (and, as a corollary, good design) embraces these aspects of sustainability is not. In practice, this concept can have several interpretations, ranging from not buying products made affordable only because they are produced by people who are not paid “living wages” to adopting social programs and design approaches like those of the Rural studio, the Make It Right Foundation, or Architecture for Humanity, which promote “design for the other 90%.”
This also brings us back to the fundamental question of what sustainable design is and what it’s goals are. The classic definition of sustainable design actually derives from a United Nations committee’s description of sustainable development. Substituting “design” for “development” in their definition, we get “design that meets human needs while preserving the health of planetary life.” A balancing act, in other words. How do we provide for ourselves now without destroying the ecosystems that will enable future generations to survive? What, then, does the goal of sustainability mean? Is it a useful term in communicating the intentions of ecodesign? What are our goals? The most basic of goals is to survive. Chances are that your primary survival needs – food, water, air and sleep – are pretty well fulfilled. Once these are assured, the objective becomes providing the means to continue to survive. The conventional precepts of ecodesign involve setting the stage so that the things we need for survival are not in short- or long-term jeopardy. The loops are closed, and we take no more from the environment than can be returned or renewed.
But we need to question whether sustainability is truly our ultimate goal. If we define sustainability as the means to continue to exist, is that really a sufficient aspiration? Many would argue that our reasons for existence, both as individuals and as a species, go beyond this to fulfilment in interpersonal or community or intellectual or spiritual senses. This state of fulfilment might best be termed flourishing and raises the accompanying question: how does design enable us not merely to sustain but to flourish?
If sustainability is not an adequate goal, what should we call this? What term could describe the attempt to go beyond “being less bad” and beyond “mere” sustainability to get to a point where design is not just minimizing negative effects but is encouraging positive impacts? There’s no consensus on this so far. One way to describe it might be “positive design,” defined as the creation of an object or system that contributes to the fulfilment of real human needs while preserving or complementing the natural world.
This definition is not earth-shatteringly different from the one we started with, but it modifies two things. It refers to “real” human needs in order to differentiate needs from wants (flourishing would be a need; a larger television would be a want). In relation to architecture, this might mean addressing social and equity issues (such as the needs of low-income groups) or, on another level, analyzing the nature of the spaces we create, looking at what they add to or how they detract from our lives.
Regenerative Design
The second modification of our earlier definition of sustainable design adds “complementing the natural world,” as opposed to simply maintaining it. The previous definition stated that the health of the planet should not be compromised but said nothing about repairing the damage that has already occurred.
This leads us to the ultimate level of ecodesign: taking care of all our current ans future needs as well as those of our planet (they are inseparable) and repairing those areas of our ecosystems that have been compromised or destroyed by human endeavours. This is no small goal in light of the demands we put on our ecosystems and the way we continue to view ourselves as separate and independent from the Earth. Examples of regenerative design (which is sometimes called restorative design), therefore, are hard to find. Some candidates include the reclamation of New York City’s former landfill into a park with restored ecosystems and the dumping of (and stripped) subway cars offshore to help rebuild coral reefs.
The Cost Issue
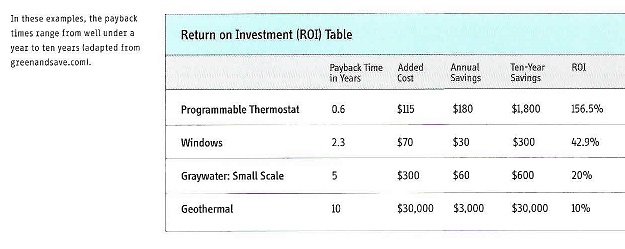
We tend to look at the case for green design in terms of avoiding negative impacts. On the flip side, we can look at the positive impacts instead. The environmental gains are often obvious. Less apparent, though, may be construction and operating cost benefits. The commonly accepted view is that green design and construction are more expensive, often prohibitively so. But more and more studies are showing that green buildings can cost the same or even less than conventional ones, providing some fundamental green design concepts are applied.
In a conventional design process, the architectural work typically occurs first, followed by engineering and then construction. Often, however, this approach results in missed opportunities because of the lack of input from and coordination with all the parties involved in the project. Integrated design is the alternative process of including all primary contributors from the beginning, before design begins. Frequently a collaborative workshop called a charrette is held, and the entire project team – including consultants, owners and contractors – meet to propose and discuss fundamental ideas. This has the dual purpose of making sure all parties are aware of hat everyone is doing and, perhaps more significantly, encouraging brainstorming in which new solutions can arise.
For example, an architect’s decision to specify triple-pane windows, which provide extra insulation but are more expensive than standard windows, will increase the construction cost. However, the specified windows will decrease the heating and cooling loads. If the mechanical engineer is involved in that decision, he or she may downsize the heating, ventilating and air-conditioning (HVAC) systems, offsetting the cost of the windows.
The new high-efficiency windows may also result in future savings in the form of lower utility biils. In many budget decisions, though, only first costs are considered, a short-sighted approach that saves a few dollars upfront while incurring much larger costs later on. Taking the long-term view, though, is especially difficult in cases where the building will be turned over to someone else after completion or when the occupant rather than the developer will be paying the utility bills. But even then, studies have shown that a building with lower operating costs will usually command a higher sale or rental price, justifying the initial costs.
Analyzing long-term costs involves looking at return on investment (ROI), sometimes referred to as the payback period. To give an overly simplified example, if installing a $20,000 solar panel leads to a saving of $2,000 per year in utility bills, the payback period is ten years. A real ROI calculation also takes into account inflation and interest rates and attempts to anticipate fluctuations in the cost of energy. Looking at the hard numbers of an ROI sometimes yields surprising results and tells us where to find the low-hanging fruit. For example, Kendall-Jackson, a winery in Northern California, has been undergoing a business-wide green conversion that examines all aspects of its operations, ranging from lighting to irrigation to pest control. The company found that many of its green programs resulted in very short-term payback periods. Upgrading their lighting to more efficient sources led to a 50 percent reduction in electrical usage and an ROI of less than a year. Better controls on landscape irrigation, combined with planting native and drought-resistant species, yielded an ROI of just two years.
Further Benefits
There are other categories of ongoing potential savings that can more than justify the price of green design. For most businesses, the costs of labor far outweigh the cost of building and operating a facility, and design decisions that result in reduced labor costs can have quite a significant effect. Many studies have shown that incorporating increased day-lighting, improved artificial artificial lighting, or better ventilation and air quality, to cite a few examples, increases productivity, decreases employee sick days, and lowers employee turnover. If the building is residential, making it healthier can create other benefits, both tangible and intangible, such as reduced medical costs and fewer days when children are home sick, keeping parents from work. We’ll look further at this in “indoor air Quality.”
Not to be left off the list of the advantages of green design are the positive effects it can have on its practitioners. It is tempting to see this new part of design as an added burden, requiring additional knowledge, coordination, time, and, if you’ve been practicing conventional architecture for a while, changes to the way you work. The other side is that it can open up unexpected paths: new clinets, fresh design influences, and increased personal satisfaction.
All told, the common perception that ecodesign is more expensive for clients and a burden for designers is more often than not incorrect. Hen ecodesign is incorporated well, e get a in-win situation in which everyone is better off. You don’t have to be a tree hugger or an altruist to incorporate green design. Green design, as it has been suggested, should just be good design.
The other misconception that we need to dispel is that ecodesign is a passing trend. Yes, we ent through this once before in the 1970s. After that energy crisis abated, after the gas lines disappeared and oil prices fell back to “normal”, the interest in conservation waned, too. Now, in the midst of what might be called the second generation of environmentalism, I think it’s fair to say that it’s not a fad this time. Very few people expect energy prices to remain low or to do anything but go up in the long term. And on the regulatory side, more and more municipalities are requiring energy- and water-efficient design. Sometimes this is just for government-owned buildings, but increasingly, codes are being updated to incorporate environmental efficiency for all buildings. Ecodesign is becoming impossible to ignore; not only is it financially wise, but it may also be required.
The above extract is from the book “Sustainable Design: A Critical Guide” from the chapter “Ecodesign: What and Why” by David Bergman and is presented here for my readers who, like me, are interested in Sustainable Design. This very good book is available on Amazon.in
Sick Business
By Dr Sumanth C. Raman
Extracts
“The National Accreditation Board for Hospitals & Healthcare Providers (NABH) was set up in 2005 to establish and operate accreditation programmes for healthcare providers in the country. The board has done some good work in this area. However, it is not mandatory for all hospitals to get certified, and the reach of the board is largely limited to hospital networks in bigger cities and towns. What about the tens of thousands of nursing homes that haven’t bothered with NABH and blatantly violate regulations? What about the NABH-certified hospitals, who do the same?
Again, the indices they put together are more related to infrastructure and are focused on the ability of the hospital to deliver care. There is no daily mechanism in place to monitor if the accredited hospitals and labs are adhering to defined protocols. A periodic inspection does little more than provide a snapshot of their infrastructure and staffing patterns, and is a far cry from being able to reliably measure care. The net result is that hospitals and labs now boast of NABH certification to tell clients that they adhere to quality standards, while all that certification does is to assess if they could deliver quality care, not if they actually do.”
“In the private sector, quality indices are often a hindrance, exposing dangerous shortcomings that need expensive solutions, and therefore need to be papered over as no hospital wants to spend a rupee more than absolutely necessary. Solutions may involve adding staff or equipment or even designating specific areas for certain activities, none of which add to the revenue of the hospital directly. Where is the incentive to invest in such measures?”
“The challenge lies in making quality profitable for hospitals instead of being the burden it is now. Hospitals see neither a compulsion nor any significant commercial value in investing in quality, and thus refrain from doing so. The only areas they are forced to invest in are those that the patients can see, like cleanliness, staff courtesy, etc.”
Fatalistic Attitude or Karma?
“It is widely acknowledged that the general quality of emerging doctors in India is not what it used to be. There are many new medical colleges, especially in the private sector, where the academic standards are not up to the mark as they just do not have enough clinical material or patients to teach the students. There are far too many students who possibly should not be in a medical school (for reasons of disinterest, parental pressure, poor academic capability, etc.) in the first place getting their degrees. The quality of the faculty is patchy at best. All this means that the doctor who emerges from such a medical school is often a health risk to the patient. Doctors in India have no legal compulsion to keep retraining themselves. They are not audited on any quality-of-care measures; it is pretty much a case of being free to do whatever one wants after the basic qualification is obtained.”
One Step Further: People/Person-Centred Care
“While the terms ‘patient-centred’ and ‘person-centred’ are used interchangeably, there is a subtle difference. When the term ‘patient’ is used, there is an unconscious shift of power to the medical professional, and this does not augur well for an equal relationship. The fundamental difference between the two terms is the purpose behind them:
- The main goal of patient-centredness is the functional life of the patient.
- The main goal of person-centredness is the meaningful life of the patient.
Why Do I BELIEVE that Hospitals Be Not for Profit?
In my opinion, an ideal non-profit would be one where:
- Doctors and staff are paid a fixed salary and are not incentivized on the basis of procedures, diagnostic tests or any other criteria.
- Tests and procedures are priced at cost, with a reasonable profit margin.
- Tariffs are standard across the institution except for room rent.
- Drugs are sold at discounted prices based on the discounts received from distributors and not at MRP.
- Support is sought from the community and corporates in the region to help sustain growth.
- Transparency is maintained across all functions and departments in the hospital.
Whatever the model considered, it is time that the healthcare industry starts to take a hard look at itself and explore alternative models of quality care delivery, and not only focus on profits. Unaffordable for the vast majority of the world, the industry has the option of voluntarily participating in the change before change is thrust upon it. After all, how long can the industry operate on the infamous catchphrase ‘Kill him if you will, but please, please bill him.’?
Are More Hospitals and Doctors Really the Solution
“It is an open secret that hospital acquired infections (HAIs) are more common in India than in the Western world. HAIs are acquired by a patient during the process of care (including preventive, diagnostic and treatment services) in a hospital or other healthcare facility. These infections can also appear after discharge. They may also be acquired by health workers during healthcare delivery and by visitors. When we think of solutions for better healthcare, the obvious answers include more healthcare providers and, of course, more hospitals. But is this really the solution? There has been a considerable increase in the number of hospitals in the last decade or so but where is the growth happening? There is also an increase in the number of medical training centres, but what is the quality of the graduates from these facilities? Has anyone done a cost-benefit analysis for this strategy?”
Risks of Hospitalization
“Hospitalization is not without inherent risks. Hospital-related infections are a real treat to patients across the globe. If a patient is admitted into a hospital for a cardiac problem and then contracts a UTI, it can be attributed to an infection acquired during or post-hospitalization.
HAIs are quite common in India but we still do not have national data for the number of infections across the country. A WHO report on HAI states:
- Out of every 100 patients, 7 in high- and 15 in low-/middle-income countries (LMIC) will acquire at least one HAI, in acute care hospitals.
- 1 in every 10 affected patients dies of HAI.
- 8.9 million HAIs occur every year in acute and long-term care facilities in the European Union/European Economic Area.
Why, Then, Do We Build More Hospitals and Medical Institutes?
In India, we still speak of hospital bed to population ratios and doctor to population ratios without taking into account changing trends in healthcare delivery. As mentioned earlier, the present hospital bed to population ratio in India is 1 bed for every 1000 people. Obviously, we need more hospitals. But we do not need more in urban areas, where the hospitals of the future are going to see fewer footfalls as smart medicine and technology keeps more patients in their homes.
We need more hospitals in underserved areas. But how do we staff these hospitals? And what good is an understaffed hospital?
One of the reasons hospitals keep getting built in India though they may be understaffed, poorly equipped and may provide an awful level of care is due to the curse of visible spending in healthcare, as we have seen in the earlier chapters. Another reason is that there are sizeable kickbacks to be made from issuing large building contracts. Everyone in the government loves promising big buildings. They can be shown to people as proof of ‘development’ in the area, and with money to be made on the side, it makes for an irresistible combination. A hospital at the best of times is a dangerous place, and a poorly staffed, ill-equipped hospital can be a killing field. Without the right personnel and equipment, they can be a treat for life. Patients are simply unaware of this. Neither the government that builds them nor the people who seek treatment there realize that big buildings with vitrified tile flooring and snazzy interiors do not mean better healthcare. Those who speak up for the ned for more hospitals point to India’s large corporate hospitals continuing to add capacity at a brisk rate. They are betting their money on hospitals staying as relevant as ever. They also point to the increasing percentage of the population that can afford better quality healthcare in India.
The silver lining for hospitals is that India is expected to have a much higher proportion of senior citizens in the coming decades. With life spans increasing and lifestyle diseases taking over from infectious diseases as the major driver of disease burden, hospitals in India still see potential for future growth.
The spoiler could be healthcare technology, where disruptive advancements can put paid to the best laid plans of hospital heads. Will the hospital as we know it today even survive in the future, say, fifty years from now?
If Not Hospitals, Then What?
Technology will continue to disrupt this sector and bring about even more radical changes in the way patient care is administered. Robotics, artificial intelligence (AI), precision medicine, telemedicine, wearable devices, data collection and sharing – these areas will continue to grow.
The homecare industry will also expand, and community care will be the future. For patients, this means lower expenses, as well as better convenience and comfort. Hospitals will save on physical infrastructure and thus will be able to utilize their resources more effectively, reducing costs significantly.
The focus will necessarily change to education rather than treatment, forcing largescale public health reforms.
As for doctors and surgeons, they will need to be experts at using technology. AI-powered tools will become the doctor’s best friend. AI can analyse reams of data and detect patterns and anomalies and suggest diagnosis options. Doctors can then interpret these and finalize the optimal treatment plan.
Of course, I am not even remotely suggesting that hospitals will cease to exist. They are an integral part of the healthcare delivery system, and a vital one at that. All I am saying is that the structures of hospitals as we know them now will change. According to a few experts, the hospitals of the future may be 80 per cent service and 20 per cent physical location.
Public Health Beyond Communicable Diseases
While we have made considerable progress in the management of communicable diseases, non-communicable diseases have emerged as the leading causes of death globally. These can include chronic respiratory conditions because of poor air quality, liver conditions due to alcohol, cancer due to tobacco usage and heart conditions and diabetes linked to unhealthy food and lifestyle. Mental health is also another neglected issue that increasingly greater attention among almost all age groups. The 2019 country report on India by the Institute for Health Metrics and Evaluation (IHME) reveals that in just ten years, NCDs have replaced communicable diseases as the top causes of death. In 2009, the three top killers were ischemic heart disease, diarrhoeal diseases and neonatal diseases. In 2019, the three top killers were ischemic heart disease, chronic obstructive pulmonary disease and strokes. This increase in NCDs has a larger impact on society. Chronic conditions lead to reduced quality of life and are an additional burden on society. These diseases are no longer the sole burden of the affluent – they affect the poorest of the poor. Why is India considered to be the golden goose for the healthcare industry? All these new patients with NCDs will need prolonged care and hence contribute to the bottom line of the industry. According to me, this is the time to step up public health activities. Raising awareness is just one part of the solution. The main part is to understand the social context of these diseases, and address those issues. The link between unclean food, air and water with diseases is well-proven. But how many towns have all of this? Every year, come winter, there is a furious debate about the abysmal quality of air in the national capital. But where are the concrete steps taken to control this situation? What about the rampant use of pesticides in food production? While there are rules in place, where are the systems to ensure adherence? A firm political will beyond just vote-catching tactics is required to stem the rot and put public health before sheer greed.
The Climate Solution: India’s Climate-Change Crisis and What We Can Do About It
Mridula Ramesh A Checklist of ActionsChecklists are a good way to quickly show the actions that are possible and desirable in building our resilience to climate change. Some actions can be taken at the individual level, some are best taken at the institutional level (for or not-for-profit, academia, etc.), and some at the policy or governmental level.
The government or policy actions are hard to get on the ground, and so the actions are ranked by an increasing perceived hardness of implementation. India is a free and fair democracy, and individuals should recognize that their slated preferences will make a difference.
Individuals
-
Choices in energy
- Use energy-efficient appliances, including LED lighting and energy-efficient fans.
- Maintain air conditioner temperatures at 24-25 degree Centigrade and clean the filters regularly.
- Paint your roof white.
- Use solar-powered DC microgrids where appropriate.
- Choices in food
- Eat less meat.
- Eat fewer dairy products.
- Avoid food waste
- Store provisions at eye-level in transparent containers and do not stack items behind one another.
- Be conscious of food waste – measure, monitor and reduce wastage. Segregate your waste. Manage wet waste locally.
- Choices in water
- Measure your water consumption – install meters at different points of use. Without this, leaks will be hard to find.
- Use a bucket to bathe, turn the tap off when you brush, get a dual-flush water closet.
- Treat your sewage, and reuse greywater to flush, or in gardens.
- Lower water pressure.
- Install a sound rainwater-harvesting system.
- Choices in transport
- Walk. If there are problems with pavements (or lack thereof), waste and dogs, talk to your councillor.
- Try carpooling.
- Try to take public transport for longer distances. For the economically privileged and time-starved, taking public transport is seen as being inconvenient, uncomfortable and low-status. The first is a myth if we equate convenience with time.; the second can be dealt with through cleaner and air-conditioned public transport options; and the last can only be solved by changing your thinking.
- Check and maintain optimum tyre pressure and service your vehicle regularly and maintain the appropriate gear for a given speed while driving.
- Choices as a citizen
- Understand the social contract and your role in propagating or changing it.
- Before believing any news, look for data from reputed sources.
- Vote and talk to candidates on issues. Democracy is NOT an armchair sport.
- Beware of tokenism: Putting a ‘like’ on social media for an action taken by someone else is insufficient.
- Believe that your actions matter. As a Tamil saying goes, ‘siru tuli, peru vellam’ – small actions can lead to a flood. It requires us to believe our actions can make a difference and take the first step.
Institutions
- Corporate citizenship
- Participate in public-private partnerships in building climate resilience – managing waste, water and improving tree cover, to name just three avenues of action. Smaller companies can do it on a smaller scale in their immediate neighbourhoods.
- Use your CSR and work with the government to ensure access to government schemes for disadvantaged populations.
- Enlightened self-interest
- Climate change is arguably the greatest disruption of our time. Mainstream climate-change thinking into your strategic process.
- Buyers of agricultural commodities in the sectors of FMCG, sugar, cotton-spinning, animal feed and animal products: Act as a bridge to bring different groups (academia, financiers, input suppliers) to the farmers doorstep to improve their resilience.
- Internally price water, waste and carbon – our experience shows that it will add to your bottom line. Genuine action in water, waste, energy is better than tokenism for your reputation.
- Take full ownership of the packaging of your products, including reverse logistics and management.
- Adopt forests and increase tree cover within your campus.
Government
- Open up urban waste management to the private sector: mandate bulk generators of waste (apartment complexes, offices, factories, hospitals, academic institutions) to go zero-waste, or manage waste in-house. Give high priority to schemes like Swachh Survekshan that emphasize process, progress and foster healthy competition between cities.
- Accelerate the creation of a national agricultural market by investing in grading procedures (including improving the trustworthiness of the grader), improving storage, transport and finance facilities for small farmers. Enabling technology and increasing competition between buyers can help shift the equilibrium to one that is fairer to small farmers. Make concerted and focused attempts to successfully pilot and grow Farmer Producer organizations.
- Institute a congestion tax for central business districts and use the receipts to fund public transport, and/or develop walking and cycling infrastructure. Parking fees should also be used tactically and strategically to reflect the preference for public and non-motorized transport.
- Adopt a universal carbon tax and return all proceeds to citizens equally. India already has this in several pockets, including excise duty on petrol and diesel, and cess on coal. The tax-net and method, either implicitly or explicitly, needs to cover other forms of carbon emissions.
- While there is already a regulation requiring manufacturers to be responsible for their packaging waste, including post-consumer waste, there needs to be an emphasis on uniform enforcement of this rule.
- Explore the replacement (partially to begin with) of subsidies for fertilizer, food and agricultural credit with a universal basic income (UBI). Many of those subsidies may not reach the smallest of farmers, who may be better reached, and made more resilient, with a UBI.
- Understand the magnitude of virtual water export embedded in our livestock, animal product and other agricultural exports. Institute a water cess on these exports to prevent free donation of our virtual water to other countries. Use the returns from this cess as part of the UBI for rural households.
- Ensure up-to-date, accurate, easily available data. The lack of timely, relevant and accurate data is one of the biggest impediments to meaningful, effective and inexpensive action.
- Tighten directed priority-sector lending to small and marginal farmers: The JAM trinity and loan-size norms (priority sector loans should be no greater than a given amount per farmer) can be used to ensure that credit really reaches the small and marginal farmer.
- Keep forests sacrosanct. As hard as this will be to do so, strong forests are the strongest weapons in our arsenal to build climate resilience.
- Implement a universal water price. Since water and its pricing is a state subject, this is necessarily a state decision. That is a good thing. Drier states like Rajasthan and Tamil Nadu, with probably greater voter support, can make a beginning and pave the way for other states. While a water price may be difficult to stomach, pricing electricity for farmers (with a refund given to the smallest farmer for judicious usage) is a more palatable choice. This is also smart politics: Gujarat and Madhya Pradesh have voted their incumbents back to office because of strong water governance that included pricing electricity for farmers.
- Institute common ownership of groundwater. A water price is meaningless unless users pay for water drawn from below the ground. Use the next drought to institute common ownership of groundwater – never waste a crisis!
COVID-19:Coverage + Resources
https://www.healthcaredesignmagazine.com/trends/perspectives/covid-19-coverage-and-resources
Healthcare Design will continue to monitor the situation with an eye on design and the built environment, and the role each plays in how the pandemic is managed.
Here, you’ll find an updated list of COVID-19-related articles and news items as we publish them. Additionally, we’ve compiled archived content from Healthcare Design on topics including infection control and prevention as well as biocontainment.
Riverstate Hospital-PortHarcourt-Nigeria:AutoCAD Plans
Download
SPACEMED-Quick Calculation Template
Download
SPACEMED-Planning Templates
Download
SPACEMED-Essentials
https://blog.spacemed.com/
Online Healthcare & Medical Courses –FutureLearn
https://www.futurelearn.com/subjects/healthcare-medicine-courses
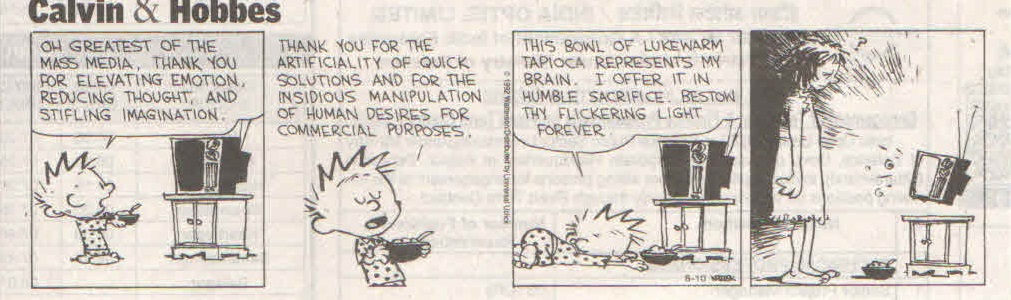
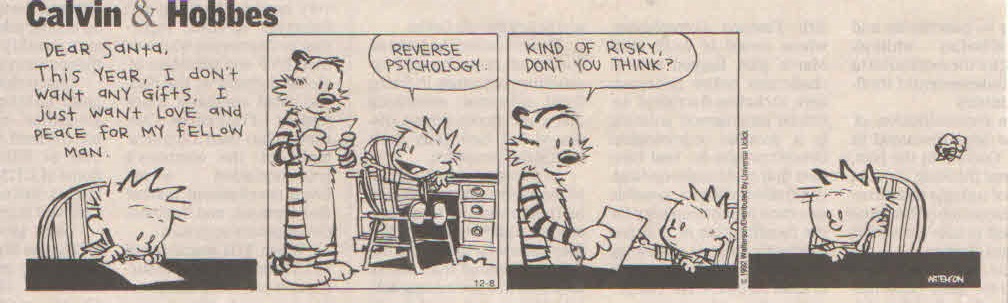
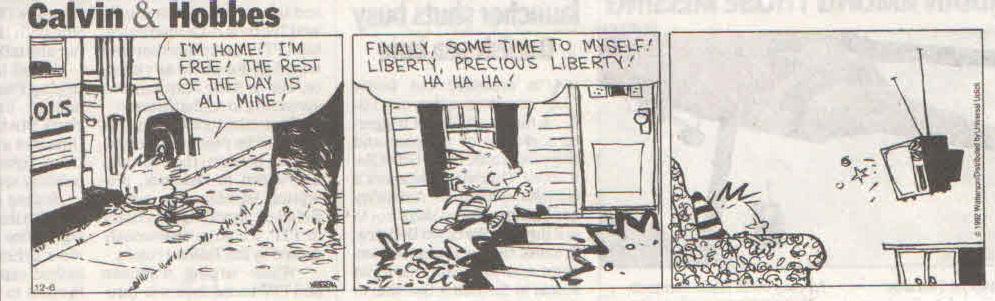

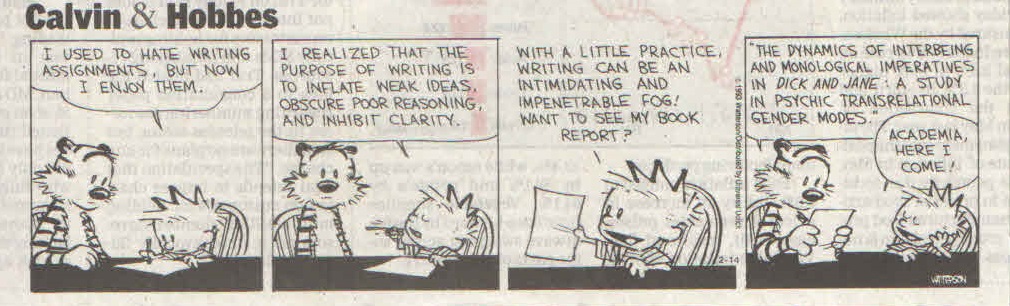
These are some of my favourite musicians and here they sing about my life and beliefs.
Mountain Jam – Duane Allman
They Call Me the Breeze – J.J. Cale/Eric Clapton
Flying Without Wings – Westlife feat. BoA
Ripple – Dead & Company
Stuck in a Moment You Can’t Get Out Of – U2
Free Bird – Lynyrd Skynyrd – Live
Walk Tall –John Mellencamp
Wasted On The Way – Crosby, Stills and Nash
The Road to Hell – Chris Rea
Shine On You Crazy Diamond – David Gilmour
Lives in the Balance – Jackson Browne
I am a Patriot – Jackson Browne
Just Older-Bon Jovi
Come Undone- Robbie Williams
Child of the Universe – Barclay James Harvest
Hospital Design Guide: How to get started
The Architecture of Health:Hospital Design and the Construction of Dignity
Michael P. Murphy Jr. with Jeffrey Mansfield and MASS Design Group
Inpatient Floor Plans
The design process for a hospital starts with the layout of the inpatient floor plan (to put it simply; you will need at least a tentative mental picture of the diagnostic, therapeutic, interventional and building services floor plans as well.)
The below extract is from the book “The Architecture of Health: Hospital Design and the Construction of Dignity” by Michael Murphy Jr. and Jeffrey Mansfield and MASS Design Group and is presented here for my Healthcare Architect readers. This very good book is available on Amazon.in at a reasonable price. Please buy and read it.
Building Type Basics For Healthcare Facilities
On The Design Of Inpatient Care Facilities
Michael Bobrow and Julia Thomas
The below extract is from the book “Building Type Basics for Healthcare Facilities” from the chapter “On The Design of Inpatient Care Facilities” by Michael Bobrow and Julia Thomas and is presented here for my Healthcare Architect readers. This very good book is available on Amazon.in at a reasonable price. Please buy and read it.
Typical Inpatient Room Plans: Outboard Toilet
Nadia
B.Arch Thesis Project
College of Engineering, Trivandrum, India
This outboard toilet configuration has the following advantages:
- It enables much better supervision by the nursing staff, as a glass pane in the door will enable nurses to check on the condition of the patient. The nurse can see the patient’s head without entering the room, which the inboard toilet does not allow. The patient(s) is not disturbed by the nurse entering the room, and also reduces the amount of time the nurse spends on checking the patient.
- The toilet and the recessed, shaded window will reduce the heat loss through the external wall in the case of an air-conditioned patient room. If the room is not air-conditioned, they will prevent heat gain through the external wall, passively cooling the room .
- The outboard toilet enables better ventilation and plumbing.
- It enables a planter (which could house potted plants) and two vertical walls that could be used for a vertical garden, considerably improving the view in the majority of cases. These views of greenery have been proved to assist in the healing process, and can reduce the ALOS (Average Length Of Stay) by up to one day.
- The planter can be maintained by giving access through a service door. The window and this door can be key operated, and can be opened by staff in good weather, patient condition permitting.
- This outboard toilet design solution will address adverse weather events such as heat waves and heavy rainfall/tropical storms, both of which may cause a prolonged electricity outage.
- It will also cut down on the consumption of electricity, which is a major cost for healthcare facilities.
Typical Inpatient Room Plans: Outboard Toilet AutoCAD Drawing
Download
Zen and the Art of Motorcycle Maintenance: Extract
By Robert M. Pirsig
‘Peace of mind isn’t at all superficial to technical work. It’s the whole thing. That which produces it is good work and that which destroys it is bad work. The specs, the measuring instruments, the quality control, the final check-out, these are all means toward the end of satisfying the peace of mind of those responsible for the work. What really counts in the end is their peace of mind, nothing else. The reason for this is that peace of mind is a prerequisite for a perception of that Quality which is beyond romantic Quality and classic Quality and which unites the two, and must accompany the work as it proceeds. The way to see what looks good and understand the reasons it looks good, and to be at one with this goodness as the work proceeds, is to cultivate an inner quietness, a peace of mind so that goodness can shine through.
I say inner peace of mind. It has no direct relationship to external circumstances. It can occur to a monk in meditation, to a soldier in heavy combat or to a machinist taking off that last ten-thousandth of an inch. It involves unselfconsciousness, which produces a complete identification with one’s circumstances, and there are levels and levels of quietness quite as profound and difficult of attainment as the more familiar levels of activity. The mountains of achievement are Quality discovered in one direction only, and are relatively meaningless and often unattainable unless taken together with the ocean trenches of self-awareness – so different from self-consciousness – which result from inner peace of mind.
This inner peace of mind occurs on three levels of understanding. Physical quietness seems the easiest to achieve, although there are levels and levels of this too, as attested by the ability of Hindu mystics to live buried alive for many days. Mental quietness, in which one sees no wandering desires at all but simply performs the acts of life without desire, that seems the hardest.
Zen Buddhists talk about ‘just sitting,’ a meditative practice in which the idea of a duality of self and object does not dominate one’s consciousness. What I’m talking about here in motorcycle maintenance is ‘just fixing,’ in which the ideas of a duality of self and object doesn’t dominate one’s consciousness. When one isn’t dominated by feelings of separateness from what he’s working on, then one can be said to ‘care’ about what he’s doing. This is what caring really is, a feeling of identification with what one’s doing. When one has this feeling then he also sees the inverse side of caring, quality itself.
I think that if we are going to reform the world, and make it a better place to live in, the way to do it is not with talk about relationships of a political nature, which are inevitably dualistic, full of subjects and objects and their relationship to one another; or with programs full of things for other people to do. I think that kind of approach starts it at the end and presumes the end is the beginning. Programs of a political nature are important end products of social quality that can be effective only if the underlying structure of social values is right. The place to improve the world is first in one’s own heart and head and hands, and then work outwards from there. Other people can talk about how to expand the destiny of mankind. I just want to talk about how to fix a motorcycle. I think that what I have to say has more lasting value.’
Reflections on Architectural Design – Drawing: Making Love to the Paper
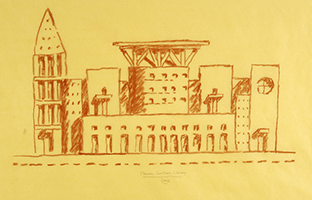

The act of drawings seems particularly important to many designers.I actually find it hard to think without a pen in my hand and at least four more inmy pocket. The act of making marks on paper mediates the flow of words. Donald Schon has referred to the architect as ‘having a conversation with his drawing’. This seems to be what Denise Scott Brown, the wife and professional partner of the architect Robert Venturi, means by the ‘eye re-interpreting what the hand has done’. The drawings designers make while thinking are frequently diagrammatic in the sense that they are not attempting to indicate three- or even two- dimensional form. Even organizing the brief is a graphically aided activity for Herman Hertzberger, architect and editor of the highly influential Dutch architectural magazine, Forum. I make notes during meetings in the form of little doodles, an attempt to use even text artistically, often switching between black, red and blue felt pens. With felt pens you can stroke the paper, a feeling akin to touching your mistress when the drawing is going well. Like I said.
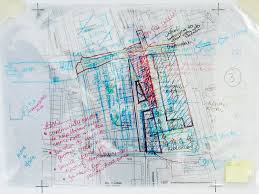
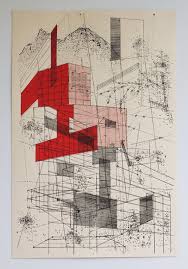
Frequently, drawings are overlaid and mixed together. Two-dimensional plans or sections can be seen with sketches and more diagrammatic marks all on the same piece of paper in what appears to be a confusing jumble. (Remember the ‘juggling’ of issues in the previous article?) Richard MacCormac (him again?) talks of his “thinking pencil”. It is definitely true that designers need to draw in order to think, and perhaps we could conclude that a failure to draw might indicate a gap in thought. The drawings I make while thinking define the problems I find and thus are related to the problems I solve. These are serious drawings, lean and mean, they try to clarify and communicate. They are not drawings as in ‘art’. At least I try not to let them become that. Many times I am have been guilty of being seduced by the drawing to the point of designing the drawings itself rather than the object it represents. Just having fun. My felt pens are almost a part of me, I travel with them, the relationship is close, very natural, such a contrast to my awkwardness with people. I love my felt pens.

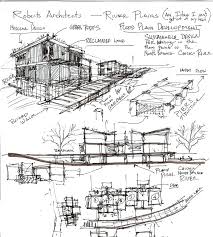 Richard MacCormac (I can hear you going: tch!) makes explicit reference to the role of the drawing tool as a way of mediating an appropriate cognitive phase. “These different frames of mind involve different instruments for producing and representing what you are doing.” What this suggests is that somehow the feel of the instrument in the hand and the way it interacts with the paper induces the right mental set. Marshall McLuhan taught us that the “medium is the message”, but for designers it seems that the medium is related to the frame of mind. (I am most at peace and very tranquil when I have a yellow ochre felt pen in my hand.) There is a sense of immediacy about drawing lines on paper that I think only a designer or an artist can feel.
I like designing most of all on white A2 paper on a writing table. No backs of envelopes during plane journeys for me, I like to design in comfort and let the drawing breathe. No standing at drafting tables either, had enough of that, I’ve paid my dues. It’s only about having fun from now on, stroking and getting stroked. Hussain Varawalla, Senior Fun-Lover, HOSMAC (India) Private Limited, Mumbai.
This is the way I like to do it:Just like that.
Richard MacCormac (I can hear you going: tch!) makes explicit reference to the role of the drawing tool as a way of mediating an appropriate cognitive phase. “These different frames of mind involve different instruments for producing and representing what you are doing.” What this suggests is that somehow the feel of the instrument in the hand and the way it interacts with the paper induces the right mental set. Marshall McLuhan taught us that the “medium is the message”, but for designers it seems that the medium is related to the frame of mind. (I am most at peace and very tranquil when I have a yellow ochre felt pen in my hand.) There is a sense of immediacy about drawing lines on paper that I think only a designer or an artist can feel.
I like designing most of all on white A2 paper on a writing table. No backs of envelopes during plane journeys for me, I like to design in comfort and let the drawing breathe. No standing at drafting tables either, had enough of that, I’ve paid my dues. It’s only about having fun from now on, stroking and getting stroked. Hussain Varawalla, Senior Fun-Lover, HOSMAC (India) Private Limited, Mumbai.
This is the way I like to do it:Just like that.
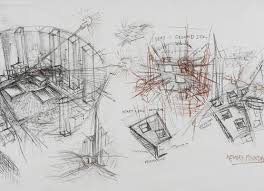
Reflections on Architectural Design – Speed of Working: ‘Capturing the Violence of the Idea’


The French designer and architect, Philippe Starck, has a reputation for working extraordinarily quickly. He claims that while travelling by plane on one occasion he designed a chair during the period the seatbelt signs were on for takeoff. He says working at this speed allows him to ‘capture the violence of the idea’.
In my experience of plane journeys, when the seatbelt signs are on for takeoff, the only thought in my mind is that of the discomfort and boredom of the journey ahead. Mr. Starck must be travelling first class, a design opportunity I have yet to experience. Having said that, I too subscribe to the idea of the design process at its best happening in a creative rush. I recently described the experience to a client (a psychiatrist) as akin to a cocaine trip. I think it made him just a little bit nervous as to who was (or would be) using whose professional services. Also, I get impatient and thus upset with the good people who give me drafting support at times like this, as the process of drawing never seems to keep pace with the sped at which the design pours out. Many times I have to apologize at the end of the day, when the dust has settled down, for any inadvertent offence given (but never taken, I think).
It is commonly held that creative work is characterized by periods of intense activity interspersed with times of quieter, more reflective contemplation. I confirm this as being my experience too. Some architects have described the periods of intense activity as being like juggling. They speak of the need to oscillate very quickly between the many issues with which an architect must be concerned. To take your mental eye off any of these issues is the equivalent of dropping a ball. This kind of concentration is extremely intense and difficult to maintain for long periods. I agree. Every evening I feel the need to contemplate seventies and eighties rock and roll, best seen through the bottom of a glass.

 As Richard MacCormac (of MacCormac, Jamieson and Prichard, Architects, fame) puts it “one couldn’t juggle slowly over a long period”. This analogy, I think, describes the skill perfectly. I have found this to be one of the skills young architects find most difficult to acquire. However, they excel at endlessly debating within themselves a minor facet of the design. Each to their own, as I have always said.
As Richard MacCormac (of MacCormac, Jamieson and Prichard, Architects, fame) puts it “one couldn’t juggle slowly over a long period”. This analogy, I think, describes the skill perfectly. I have found this to be one of the skills young architects find most difficult to acquire. However, they excel at endlessly debating within themselves a minor facet of the design. Each to their own, as I have always said.
Richard Burton, of the architectural firm Ahrends, Burton and Koralek shares this view. He feels the design process must work very quickly, this follows from his insistence that no one aspect of the problem should dominate. From his teaching and examining experience he identifies a failure to work quickly enough as one of the problems facing students trying to develop their own design process.
Michael Wilford, (previously James Stirling’s partner) refers to the “skill of prioritizing the stages at which certain inputs are valuable as distinct from an impediment to the process”. Creative inputs on design issues when construction documents are being prepared are not always welcome to those preparing the construction documents, and these fine people too are critical to the overall scheme of things, and must be kept happy. It’s not just about juggling, but also about knowing which balls to use, and when!
There is also the need to contrast the intensity of working in the group within the office with quieter periods of solitary contemplation. The need for longer periods of quiet reflection as well as the intense periods explains why the design process cannot be hurried and compressed without considerable loss of quality. Certainly, it has not been my experience that the quickest and cheapest design process will give rise to the most desirable result. Imagine trying to juggle too many eggs too fast. Undesirable results!.
In fact, bearing in mind the small part of the total cost of a building that goes on the design process, this is an entirely fallacious and counter-productive notion!
Dr Santiago Calatrava, one of an extremely rare breed of architect-engineers (he studied architecture at the Escuela Tecnica Superior de Arquitectura de Valencia in the Spanish region of Valencia and then moved to Switzerland to study civil engineering in Zurich), believes that design should have a ‘freshness and spontaneity’. He says this comes from working rapidly and intensively at certain stages of the design process. He talks about the tensions between the intense and relaxed periods of design and the need to fight for the idea and yet allow criticism of it. On the one hand it needs a lot of spontaneity and on the other it needs perseverance.’
Dr Calatrava has been awarded the Gold Medal by the Institute of Civil and Structural engineers. Way to go, Doctor! They need to be shown the light.

 Although Dr Calatrava is undoubtedly a great artist and his work is highly personal he is not frustrated, as might be expected, by a process which necessarily involves so many other people. He thinks the architect should transmit a vision of something. I think it is very much about seeing and showing the Path, the Way, something like Gautama Buddha. Great design is about seeing the Light. And it not like it needs to be approached with the seriousness of a religion. As I have said before, and intend to keep saying, it is all about having fun.
Although Dr Calatrava is undoubtedly a great artist and his work is highly personal he is not frustrated, as might be expected, by a process which necessarily involves so many other people. He thinks the architect should transmit a vision of something. I think it is very much about seeing and showing the Path, the Way, something like Gautama Buddha. Great design is about seeing the Light. And it not like it needs to be approached with the seriousness of a religion. As I have said before, and intend to keep saying, it is all about having fun.
The Boss, Bruce Springsteen, wrote a song called ‘Blinded by the lIght’. Somewhere in the middle it goes like this: “Mama always told me not to look into the sights of the sun…” There is a pregnant pause in the music, and then the next line goes: “Woah but but Mama-a-a, that’s where the fun is…” The refrain goes “Blinded by the light…” Oh well, that’s neither here nor there. It’s just a casual aside, lyrics from a song I heard years back. Our circumstance has changed since then. Do you think half-forgotten rock ‘n roll lyrics can define a vantage point from which to view the world? The first ten appealing answers will get their originators a CD of the Grateful dead titled “American Beauty” (American Reality?) as a prize. So think hard. To get back to mr Calatrava, he too speaks of the idea being not inside but outside him as some sort of distant light which offers a focus for the process. For him the design is largely linear. He does not normally believe in exploring alternatives and seems to arrive at the basic idea of a scheme fairly early on. For him this starting point can be remarkably fundamental. “Sometimes it is just a gesture or an idea about equilibrium, for example.”
I like to think that maybe sometimes it could be a funny thing that happened to him on his way to the office, for example.

 Santiago Calatrava then represents a fusion of the worlds of the civil engineer and the architect. He claims that his imaginative structures do not necessarily cost more to build but admits they might take longer to design. He feels that to design too quickly and to look for the cheapest solution is both short-sighted in that this can destroy important landscapes, and is often not an economical policy in terms of lifecycle costs. Most of his work has been commissioned by public authorities who have been convinced by these arguments.
Santiago Calatrava then represents a fusion of the worlds of the civil engineer and the architect. He claims that his imaginative structures do not necessarily cost more to build but admits they might take longer to design. He feels that to design too quickly and to look for the cheapest solution is both short-sighted in that this can destroy important landscapes, and is often not an economical policy in terms of lifecycle costs. Most of his work has been commissioned by public authorities who have been convinced by these arguments.
What I think he is saying is that you can make a good omelet without necessarily breaking (or juggling) a whole lot of eggs, if you do it with care and cook it over a low flame. Present and potential clients please note. Let us designers simmer.
Healthcare Architecture (as seen through) Ian Ritchie’s Eyes
 Ian Ritchie was born in Hove on the south coast of England. He studied architecture at the Polytechnic of Central London where he graduated with distinction in1972. He worked with a number of prominent architects, and in 1981 he formed Ian Ritchie Architects and co-founded the special design engineering firm of Rice Francis Ritchie (RFR) in Paris. Peter Rice is an engineer, and Martin Francis is an industrial designer and naval architect.
Ian Ritchie was born in Hove on the south coast of England. He studied architecture at the Polytechnic of Central London where he graduated with distinction in1972. He worked with a number of prominent architects, and in 1981 he formed Ian Ritchie Architects and co-founded the special design engineering firm of Rice Francis Ritchie (RFR) in Paris. Peter Rice is an engineer, and Martin Francis is an industrial designer and naval architect.
Ian Ritchie’s attitude towards the size and organization of his design office sounds very simple. He claims this is about the number of people who can basically communicate well together’. The number five figures strongly in his calculations. He feels groups of up to five work well on a design.To cut short the story, the result is a staff of 20 to 25 people who, as lan says ‘can actually all discuss around a table, especially when someone has a birthday’.
Heading the architectural design section of a healthcare consulting firm as I am, I too feel that smaller groups of people work better and with more intensity. Alienated as I am, there is actually only one person in the firm with whom I can communicate well (or rather excellently). S/he is not even an architect, not the big boss and not even one of my fellow directors. Odd, to put it mildly. Eccentricity is flaunted by many designers, and not only in their designs. My designs are anything but eccentric, models of rationality, rather. It’s more the clothes I wear and the company I keep. Anyway,

 Robbie Williams sings in his song Better Man.
Robbie Williams sings in his song Better Man.
“. ..and I’m doin’…the best I can…to be a better man.” No surprises there. I too am trying to improve the quality of my wardrobe. I bought four long sleeved shirts one of which can be best described as ‘funky cool’, but what the hell, three out of four ain’t bad.
Why are we singing along with Robbie and discussing my laundry? This article is supposed to be about healthcare architecture seen through Ian Ritchie’s eyes. Let’s pay that some lip service, at least.
For Ian the design process begins with an attempt to construct a working relationship with the client. Before even discussing architecture, he tries to lead his client into his process. He says:
“It is very rare for a client to commission a building more than once in his life, except in the commercial sector. There is nobody who ever trains or deal with an architect. The first move is to talk through the brief, understand what has led to it, understand fundamentally what it is about.”
For me the design process begins with trying to find the time to design the damn thing .My clients are usually financiers and/or doctors wanting to build corporate hospitals, and the brief is easy to understand, fundamentally it is about making money through providing healthcare services. Jokes apart, that is more easily said than done. Financial planning has to precede any ideas about buildings. When I look at rows of figures they seem to be dancing to some kind of presumably divine music, so obviously I am only marginally involved in doing this financial planning. Fortunately for our clients there are good people in the firm who do this very well.

 Technology is an important factor in the financial planning and the architectural design of healthcare facilities. Ritchie, however, does not feel that technology is a design generator for him. He has clearly been asked about this before and describes his relationship with technology thus:
Technology is an important factor in the financial planning and the architectural design of healthcare facilities. Ritchie, however, does not feel that technology is a design generator for him. He has clearly been asked about this before and describes his relationship with technology thus:
“When people ask me this question I use an analogy. I describe this beautiful parrot sitting on my shoulder — multicolored, very beautiful – called ‘technology’. Very often he leaps off the shoulder onto the paper and shits all over it before we’ve actually started thinking and you have to get hold of him and stick him back up here. He is tame, he does behave himself and he doesn’t always end up in the project at all, but he’s there and wet talk to him all the time.”
All I can say is it’s a good thing he jumps onto the paper to do his thing, otherwise we would be discussing lan Ritchie’s laundry along with mine, and his would not be ‘funky/cool’.
What does healthcare architecture have to do with beautiful parrots doing what they do? I’ll try to tell you. Technology can indeed do what the parrot with the same name does to your best laid plans for your healthcare facility, unless tamed. C T Scans are to be thought of as machines that help diagnose illnesses in much the same way your GP takes your pulse, and not as ravenous monsters that demand to be fed with warm bodies. The architecture, the interior design and the people the patient meets on his way to this monster need to be as reassuring and generate the same warmth and concern as the pulse-taking GP. Ian is right about that, and very well put too, he has a way with words, some people do. It’s an acquired gift.
Ian has a parrot on the other shoulder too:
“There’s a little one on the other shoulder called ’art’ or poetry’, he’s very powerful squeaks a lot but he’s not got the nerve of this one yet and that’s because we are still maturing into that field. It’s only been a few years since we’ve been working hard at it, so it doesn’t feel comfortable yet.“

 That parrot’s also called ‘funky/cool’ and whenever I wear one of the funky/cool selections available in my wardrobe s/he sits on my shoulder too. Doesn’t shit on the paper or create laundry. S/he’s a parrot that is chilled out and we need Robbie’s help again in describing how s/he makes me feel:
That parrot’s also called ‘funky/cool’ and whenever I wear one of the funky/cool selections available in my wardrobe s/he sits on my shoulder too. Doesn’t shit on the paper or create laundry. S/he’s a parrot that is chilled out and we need Robbie’s help again in describing how s/he makes me feel:
“…so high you’ll be flyy..yyy…ing!” From his song titled She’s the One.
For Ian Ritchie it is the technology or function of the building which brings order to the art or poetry. For me it is music that brings order to my life. Living an orderly life then enables me to bring to bring technology, art, function (poetry?…working hard at it…) and above all order to my healthcare facility.
In conclusion, if you’re trying to design a healthcare facility (or, for that matter, any kind of building) attempt to keep bird-shit off your paper. Keep both parrots on your shoulder, where they belong.
And, you know, if either of them has just gotta go, it’s only laundry, after all.
Reflections on Architectural Design: The Central Idea
The ‘Central Idea’: Hang On To It Like Grim Death!

 Good designs often seem to have only a few major dominating ideas which structure the scheme and around which other relatively minor considerations are organized. Sometimes they can even be reduced to one idea known to designers by many names but most often called the ‘concept’ or the ‘parti’. Such ‘central ideas’ inevitably emerge from early design explorations into the project.
Good designs often seem to have only a few major dominating ideas which structure the scheme and around which other relatively minor considerations are organized. Sometimes they can even be reduced to one idea known to designers by many names but most often called the ‘concept’ or the ‘parti’. Such ‘central ideas’ inevitably emerge from early design explorations into the project.
In architectural design in general, these dominating ‘central ideas’ usually can be visualized almost immediately in terms of one or more kinds of architectural form(s) or architectural space(s). The ‘central idea’ for a healthcare (especially hospital) project may, however, be of a more complex nature, not so easy to grasp and not so easily visualized in architectural form or space. The ‘concept’, for a hospital building may involve elements of its proposed manner of financing, it may involve a separate ‘central idea’ about a building services framework which the designer, so to speak, can hang his hat on, and, in addition to the usual social and formal concerns will definitely involve an idea of the evolution and change of the building through a long time span.
 In HOSMAC, we approach our projects ‘holistically’. We insist on our clients formulating a ‘statement of intent’ for the project. This forms a reference point for professionals of various disciplines working on the project to make decisions consistent with the project goal. Thus we see that this ‘central idea’ need not restrict itself to the process of architectural design. A.N. Whitehead in his presidential address to the Mathematical Association puts it rather succinctly:
In HOSMAC, we approach our projects ‘holistically’. We insist on our clients formulating a ‘statement of intent’ for the project. This forms a reference point for professionals of various disciplines working on the project to make decisions consistent with the project goal. Thus we see that this ‘central idea’ need not restrict itself to the process of architectural design. A.N. Whitehead in his presidential address to the Mathematical Association puts it rather succinctly:
“The art of reasoning consists in getting hold of the subject at the right end, of seizing the few general ideas that illuminate the whole, and of persistently organizing all subsidiary facts around them. Nobody can be a good reasoner unless by constant practice he has realized the importance of getting hold of the big ideas and hanging on to them like grim death.”
Time and again, however, I have been involved in projects where the client has a clouded vision of what it is he or she wishes to achieve, and this fogginess communicates itself to all those who are involved in the project, there is no ‘central idea’, there is no clarity of vision. And of all the various professionals involved I think it is the designers who feel the most frustrated by the aimlessness of the exercise.

 Designers need to feel purpose.
Designers need to feel purpose.
The architect Richard MacCormac of the firm MacCormac, Jamieson & Prichard, referring to the ‘big idea’ keeping designers going through what he recognizes as a very fraught process, says:
“This is not a sensible way of earning a living, it’s completely insane, there has to be this big thing that you’re confident you’re going to find, you don’t know what it is you’re looking for and you hang on.”
Somebody at the top has to communicate to the whole team that yes, there is a pot of gold at the end of this rainbow. This sense of purpose is what sustains the team, the quality of the idea is the sustenance that nourishes and keeps the team going towards this distant light, sometimes maybe hazy but definitely beautiful.
Reflections on Architectural Design: (and The Dynamics of Design Teams)

 In the organization HOSMAC (India) Private Limited I head the architectural design section and what follows are some of my reflections on design in general and the dynamics of design teams in particular.
In the organization HOSMAC (India) Private Limited I head the architectural design section and what follows are some of my reflections on design in general and the dynamics of design teams in particular.
I feel that the interaction between members of a design team can be a very important influence on the design process.
To quote Richard Burton, of the architectural firm of Ahrends, Burton and Koralek:
“The group has a distinct advantage over the individual because ideas can become personal property or one’s own intellectual territory. The strength of that territory is considerable, and the difficulty of working alone is often in the breaking of the bonds caused by it. With a group the bonds are broken more easily, because the critical faculty is depersonalized.”
Burton is talking about working with his two partners, but in the process of designing a healthcare facility in our firm, HOSMAC (India), I often get insights into what I am trying to do from design team members of varying backgrounds, especially doctors and hospital management professionals. The insights they have into the operational aspects of the health care facility under design often enable me to view the issue from a completely new perspective.
In their early years of working, Ahrends, Burton and Koralek elaborated on the idea of depersonalizing the critical faculty into a strategy to maintain a freshness of view on each project. They would only allow one to make close contact with the client and one of them would remain substantially ‘detached enough to see some twist in the changes of the direction of the inquiry’.
An interesting concept, certainly, and one I would love to put into practice if I could work closely with two other designers of comparable design maturity as myself! What is happening now with us is that we turn everyone loose on the client independently, and from the resulting ‘wealth?’ of points of view and comments generated, I dredge for useful ‘intervention’ in my thought process. At any cost, stagnation in the process is to be avoided.
To quote Burton again:

 “To rely continually on common assumptions can be dangerous, not least because it can lead to stagnation, so we welcome intervention, which can be either external or from within the group…it’s essential that the group should not become a small closed community. Indeed we see closed communities as seed-beds of fantasy.”
“To rely continually on common assumptions can be dangerous, not least because it can lead to stagnation, so we welcome intervention, which can be either external or from within the group…it’s essential that the group should not become a small closed community. Indeed we see closed communities as seed-beds of fantasy.”
Different clients with vastly varying viewpoints, different engineering consultants and the different experiences of design team members on different sites ensure that we never get into a ‘design rut’ or, as Burton so aptly puts it, grow ‘fantasies’. This comment, of course, holds good for our firm beyond the sphere of an individual project, specialized as we are in the design of healthcare facilities. In fact, our relationship with each individual client is a critical factor in determining the final outcome.
As an architect, clients notwithstanding, there are elements of art in every design, which is a highly personal thing, and it may be thought the designer would feel some amount of frustration to be involved in a process involving so many other people. But is in fact precisely because the design process involves so much cooperation and communication that can make it so rewarding. There is a thrill one gets from group activity that cannot be replicated through individual effort. This particular frisson is known, for example, to those who play music in groups or are part of a sports team, and seems to come from the very fact that the group is able to perform together as a result of some understanding which they share but which may not necessarily be made explicit to others outside the group. I find this especially evident in the inner core, the key decision-makers in any project, who subscribe to a shared vision that drives them. The feeling of accomplishment at completion is all-satisfying.
At times we find the client trying to impose theoretical ideas or conclusions drawn from user research that has been conducted away from design to propose prescriptive formulae for designers to follow. To quote Burton on this:
“life is a bit more complicated than that…and working together with people can achieve an enormous amount within this jungle of difficulty’.
I too am of the opinion that user research should be conducted with the active participation of designers, preferably in the form of feedback studies on buildings designed by those same designers, to accurately measure the fit between design assumptions and the reality of an operating facility.
If the organizational structure of the design team is not very clearly defined, it can be an advantage. The architect Richard MacCormac of MacCormac, Jamieson, Prichard speaks about his role as ‘making a series of interventions at different stages of the design process’. He likes to have a degree of detachment from the everyday running of the project that allow him to intervene at what he considers to be the critical moments. (How I wish I could afford that luxury! Our design process needs my constant steering.) MacCormac says ‘Part of the game is to create a crisis by recognizing that something is not right.’ (This role we reserve for our HOSMAC (India) Director, Dr. Vivek Desai!) The design concept that emerges from one of MacCormac’s self-induced crises can revolutionize and reorganize the whole design. However, in his view, this can only be a team activity. He says:

 “I or somebody else comes up with an originating idea, some idea that seems powerful enough to generate a scheme and to subsume a lot of decisions within it…it needs someone in the team to pick up the ball and run with it. I find that I seize on somebody in the team who understands what the crisis is…you have to find this person who sees what it is about otherwise it’s hopeless.”
“I or somebody else comes up with an originating idea, some idea that seems powerful enough to generate a scheme and to subsume a lot of decisions within it…it needs someone in the team to pick up the ball and run with it. I find that I seize on somebody in the team who understands what the crisis is…you have to find this person who sees what it is about otherwise it’s hopeless.”
Unfortunately, in the HOSMAC (India) team at the present moment I am the only one in a position to see what it’s about (so it’s not hopeless, at least!). We need design team members who are in this position to see. If you have survived this article till this point, maybe it’s you! Email me at hussain.varawalla@hosmac.com, talk to me in a way that demonstrates you could maybe see. Mail me a picture of yourself in your favorite T-shirt in the position you find yourself most comfortable, so that I can see if you can.
So far in my career I have never worked behind a closed door, maybe because I never merited one! But given the choice, I would prefer to work in the midst of my design team members, keep a finger on the pulse, I want to know who’s happy, who’s sad and why. I prefer to work with architects who are young enough to be the children I never had. Usually they have no idea of what’s possible and therefore no idea of what’s impossible. The intention then being to do one ‘impossible’ thing before the first round of tea every morning.
It kick-starts the day with a satisfying roar. Go, team, go!
Reflections on Architectural Design: (and The Design Of Healthcare Facilities)

 In the organization HOSMAC (India) Private Limited I head the architectural design section and what follows are some of my reflections on design in general and the architectural design of healthcare facilities in particular.
In the organization HOSMAC (India) Private Limited I head the architectural design section and what follows are some of my reflections on design in general and the architectural design of healthcare facilities in particular.
Design as a professional activity separated from the making of things is a relatively recent phenomenon, and the trying to understand how designers’ design is a field still in its infancy. In the early years of serious design research it was fashionable to see design as an entirely generic and field-independent activity. Thus a respected worker in the field, Sydney Gregory, could confidently assert that ‘the process of design is the same whether it deals with the design of a new oil refinery, the construction of a cathedral or the writing of Dante’s Divine Comedy’. I am not convinced of this view and rather doubt that Dante would be either! It would be farfetched to compare the mindset and skills required for the design of a healthcare facility in 2011 to those required for the penning of poetry.
Architectural design is generally recognized as presenting a ‘wicked’ problem. By this is meant that such problems defy complete description and lack the clarity of formulation found in scientific problems. They are the sort of problems where the information you need to understand them rather depends on your ideas for solving them. This sort of design is a ‘knowledge-rich’ as opposed to ‘knowledge-lean’ activity. In other words, architectural design requires us to have considerable amounts of knowledge beyond that stated in the problem description. Healthcare design demands sensitivity to as diverse concerns as addressing the anxiety of a cancer patient undergoing treatment to the engineering requirements of the radiation therapy unit in which he or she is being treated. Above all one has to realize that this sort of design involving addressing such varied fields of knowledge and empathy is a process in which there will be no one recognizably correct or even optimal answer.
Early writers on the design process tended to see it as a sequence of cognitive operations conducted entirely within one brain. Such models have an almost unassailable logic and appear quite convincing to those not personally involved in the act of designing. However, while the ‘methodologists’ gathered at conferences to discuss the finer detail of such ideas, designers were quietly ignoring them and getting on with the business of design.
Today it is easy to see why these sequential models of design were doomed to failure. They began from several false premises two of which we need concern ourselves with here. These concern fallacies about the beginning and end of design: first, that design problems are, or indeed, can be stated clearly, and secondly that there are solutions, which can be considered in some way optimal. As mentioned before, today we recognize architectural design problems belonging to a type known as ‘wicked’. They are often vague expressions about a change of some kind, which is needed or desired rather than a clear statement about a totally defined goal. They should therefore most definitely not be considered to be like crosswords or other popular types of puzzle. These are characterized by a totally defined objective and usually have a single correct solution, which can often be recognized as such when it is found. Those who consider design to be merely problem solving do the field a disservice. A large part of the business of designing involves finding problems, understanding and clarifying objectives and attempting to balance criteria for success.
We have now recognized that designers often come to better understand their problems through their attempts to solve them.
Most designers are at their best when designing, rather than writing about the process they follow. Of course, we must sell our services in the marketplace and so we may not always describe our processes honestly! My many years of design experience also suggest that when I like a solution, I can be amazingly creative in imagining the ‘logical’ processes that led to that solution. Other designers too can be quite capable of denying to both themselves and others the obvious importance of issues that they have chosen either to ignore completely or to relegate to minor consideration. Depending on who is ‘driving’ the project, a doctor, an investor, a Vice-President (Projects) or a philanthropist, the frame of reference through which the decision-making process is viewed can vary greatly. The designer then has to ‘wear the hats’ of those users of the facility who are getting neglected as to their needs as well as he can, champion their interest through the design process. Further to this, architects are expected to have a social conscience, to ensure that the buildings they design are good neighbors and eco-friendly. Design has to address a multitude of issues; the designer has to put his values on the line.

 It is a reasonable assumption that clients choose architects to some extent because they like earlier designs they have seen, or, as in the field of healthcare design, because of special knowledge of the particular features of the building type. Some clients have a very clear vision of how they want the final design to be, while others may have almost no idea. Some clients are particularly concerned about some feature and care little about others. The relationship between client and designer therefore is not like an examiner setting students a question but rather more like someone needing help in a situation where many courses of action are possible.
It is a reasonable assumption that clients choose architects to some extent because they like earlier designs they have seen, or, as in the field of healthcare design, because of special knowledge of the particular features of the building type. Some clients have a very clear vision of how they want the final design to be, while others may have almost no idea. Some clients are particularly concerned about some feature and care little about others. The relationship between client and designer therefore is not like an examiner setting students a question but rather more like someone needing help in a situation where many courses of action are possible.
At its best, the interaction between client and designer can be a highly interactive and creative one.
Design is undoubtedly an artistic business, but it is dangerous to confuse it with art. Most designers see themselves as artistic but not necessarily as artists. Design usually involves making something that must work in some way as well as expressing some values or ideas. Inevitably, the end product of contemporary architectural design often demands that a great deal of technology be employed. This is especially the case in the design of today’s healthcare facilities. The extent to which the problems posed by technology influence the designer’s thoughts is a central issue in understanding the design process. Within the same healthcare facility, the architect may switch mental gears (tracks?) while designing the inpatient areas as contrasted with an Operation Theater Suite. Nowadays there is a proliferation in architectural theory and also a considerable variation in the way architects regard the role of technology in design. In healthcare facility design in the new millennium, though, architects necessarily need to understand the technological requirements of the building. The new frontiers in the delivery of healthcare through hospitals are divergent, one concerned with alleviating mental distress in the form of addressing the anxiety felt by patients and their family in highly stressful situations, and the other concerned with the frontier of designing for the engineering needs of contemporary medical technology.

 There are of course many other questions about the nature of the design process that could be posed, and the reader will no doubt have his own. The few central issues I have raised are an attempt to stimulate the mind.
There are of course many other questions about the nature of the design process that could be posed, and the reader will no doubt have his own. The few central issues I have raised are an attempt to stimulate the mind.
It becomes necessary to bring some of the issues about design raised here into sharper focus by dealing with them directly and comparing and contrasting various approaches to them. While there may be as many approaches to architectural design as there are architects, I suspect that in the healthcare design fraternity there may be more consensus on the general way forward. Being a fragment of the whole, there is likely to be more uniformity within.
For now I leave you with this thought: The great philosopher Ludwig Wittgenstein is reported to have said ‘you think philosophy is difficult enough, but I tell you it is nothing to the difficulty of being a good architect’.
These are some of my favourite musicians and here they sing about my life and beliefs.
Story Of My Life – Bon Jovi
Welcome To Wherever You Are-Bon Jovi
Last Man Standing – Bon Jovi
Peaceful Easy Feeling – Glenn Frey
Human Touch – Bruce Springsteen
Sad Café – Eagles with David Sanborn
Money Talks – AC/DC
Radio Nowhere – Bruce Springsteen
Better Days – Bruce Springsteen
Forever Young – The Band Bob Dylan
Further On Up The Road – The Band Eric Clapton
Stairway To Heaven – Led Zeppelin
Shadow Captain – Crosby, Stills & Nash
November Rain – Guns N’ Roses
Comfortably Numb – David Gilmour
Proposed Cumballa Hill Hospital at Mumbai for Dr Shetty
150-Bed Hospital at Gelephu, Bhutan.
My 99 Sq. Ft. Bedroom in Thane, Mumbai Metropolitan Region




 A corner of my living room, lamp lit
And blazing with light
A corner of my living room, lamp lit
And blazing with light
“These are some of my favourite musicians and here they sing about my life and beliefs.”
Shine On You Crazy Diamond – David Gilmour
Stairway To Heaven – Led Zeppelin
We Weren’t Born To Follow – Bon Jovi
Dream On – Aerosmith
Silver and Gold – U2
No One Said It Would Be Easy – Sheryl Crow
Steve McQueen – Sheryl Crow
Boulevard – Jackson Browne
Unwell – Matchbox 20
Doctor My Eyes – Jackson Browne
Van Diemens Land – U2
I Have a Dream – Westlife
U2 – Love And Peace Or Else
U2 – Yahweh
Lynyrd Skynyrd – The Ballad Of Curtis Loew
Work Done While At Hosmac India Pvt. Ltd. As Director-Design Services
I am in solidarity with the outstanding students and activists of India, my country, it’s all I know.
I am a Patriot – Jackson Browne
Green Design: Environmentally Effective Design Principles
HEATING, COOLING, LIGHTING
Sustainable Design Methods For Architects
Norbert Lechner
Fourth Edition – Copyright 2015 by John Wiley & Sons, Inc.
“One of the most useful and important books on building design in years…Nowhere else have we seen such clear explanations of energy flow mechanisms that occur in buildings. Take our word for it, this book is a must have for any design firm.”
Environmental Building News
A leading guide and reference on the design of a building’s environmental controls, Heating, Cooling, Lighting Fourth edition supplies architects and students with the strategies they need for making initial design decisions when creating energy sustainable buildings. Based on a three-tier approach, – load avoidance, optimum use of natural energies, and the selection of appropriate mechanical equipment – this bestselling guide gives designers the information they need when considering a buildings thermal and lighting needs in order to create aesthetic, low energy sustainable buildings.
New to this edition:
– Useful content for the “integrated design” studio, explores how strategies interact to create an integrated
building system
– Information on Tropical Architecture explains how that climate differs from design in temperate regions
– The latest practices for low energy building design
– Filled with the most recent developments, codes, standards, and rating systems for energy efficiency
– A checklist to help design low energy buildings
Well organized and clearly written, without overly technical language or mathematics, Heating, Cooling, Lighting, Fourth Edition is an essential resource for today’s architects and architecture students.
NORBERT LECHNER is Professor Emeritus in the College of Architecture, Design and Construction at Auburn University and an architect. His articles have appeared in Architectural Lighting and Solar Today, and he is invited to give lectures and workshops throughout the world. He is author of the companion book Plumbing, Electricity, Acoustics, published by Wiley.
CHAPTER 1
Heating, Cooling and Lighting as Form-Givers in Architecture
I urge you to buy and read with attention this excellent book. It is value for money and a necessary read in these days of climate crisis. It focuses on the reduction of our dependence on the use of fossil fuels.
Chapter 2: Sustainable Design and Energy Sources
Chapter 17: Tropical Architecture
Chapter 19: Checklist for Designing Integrated Sustainable Buildings
I urge you to buy and read with attention this excellent book. It is value for money and a necessary read in these days of climate crisis. It focuses on the reduction of our dependence on the use of fossil fuels.
A Project Planning Guide For Healthcare Facility Owners
By
Brian Walrath & Godfried Augenbroe
Purpose
According to a recent study, about 30 percent of US real estate projects are cancelled midstream, while more than half run up to 190 percent over budget and 220 percent over their initial time estimates. The reasons for this are manifold but poor decisions during the initiation and early planning of the project can be pointed to as one of the main causes. Most poor decision-making stems from lack of information, bad judgement, or lack of communication and transparency between what the client expects and what the project team can deliver. Proper project planning procedures and methods will lead to proper contingency planning, management of partner relationships and contracts, management of dynamic unforeseen changes and associated risks that can, and most probably will, occur in the course of the project. The role of the owner cannot be overstated in all of these targets.
As a general rule, healthcare executive leaders may have only one opportunity in their career to participate in the design and construction of a hospital replacement or major hospital expansion project. The interaction with planners, public bodies, architects, engineers and other stakeholders is a daunting prospect for which an owner organization will seek help from specialized firms that can represent the owner. This guide should allow the owner to better navigate the process. Additionally, while this guide has no intention of replacing the deep and specialized knowledge of or need for advisors (internal or external), it will prepare owners to recognize the major tasks and decision steps throughout the process, while keeping the focus on the desired outcome. Any owner should recognize that the slogan “ if you don’t know or cannot express what you want, you will not get what you need” is as true today as it ever was.
Guiding Principles for the Development of the Hospital of the Future
The Joint Commission
Introduction
Human lives weigh in the balance every day in hospitals. For hospital patients and their families, the hospital experience is often a central point in their life – where their child was born, where their beloved died, where they received life-saving treatment, rejuvenating therapy or care to overcome an episode of illness. The hospital is the setting of oft-told tales among friends and family throughout the generations. It is no wonder that hospitals are often used to depict human drama – and even comedy – for popular consumption across the panorama of entertainment media.
In reality, hospitals are the setting where cutting-edge medical advances relieve suffering, and bring healing and new life for those whom, even a few short years ago, there would be little hope. Featherweight babies, born eight weeks prematurely can now survive and even thrive. Minimally invasive surgeries allow patients to heal quickly with less risk of complication. The evolving science of organ transplantation brings a second shot at life for an increasing number of people whose lives would otherwise be foreshortened.
In addition to their impact on human life, hospitals are a major driver of the US economy. The hospital industry is the second largest private-sector employer in the US and contributes nearly $2 trillion of economic activity. In any small communities across the country, the local hospital is the largest employer and most valuable economic asset.
Consumer attitude towards hospitals waxes and wanes, seemingly with some dependence on hospital news that makes headlines, such as traumatic medical errors, rampant hospital-acquired infection, and unscrupulous billing practices. There is no doubt that hospitals face greater scrutiny over the issues that can erode public trust. In order to secure the public’s trust, hospitals will need to become highly reliable – ensuring patients’ safety, providing clinically effective care, and embodying the ethical ideal that has long been the expectation of the public.
Hospitals will have to meet the high expectations of the public and all stakeholders in an increasingly challenging environment. There are many issues with which hospitals must now contend. These include escalating healthcare costs that are no longer publicly – or politically – tenable, changing demands in reimbursement for services, demands for transparency of cost and quality data, and workforce shortages. At the same time, the conditions and care needs of hospitalized patients are more complex. The rise in patients with chronic illness, older age adults, and medical interventions and therapies, are already influencing hospitals today and that influence will deepen well into the future.
The importance of hospital-based care will not diminish in the future. However, changes in the social and economic environments in which hospitals operate, as well as medical and technological progress require hospitals to be equally transformative as the future unfolds.
There has been a hospital building boom underway – fuelled by both increasing demand for health care services, and increasingly obsolete hospital plants. Though economic conditions are expected to slow its place, the continuing investment in hospital construction offers the opportunity to remake the hospital – its design, culture and practices – to better meet the needs of patients and families and the aspirations of those that provide their care. But, unless there are principles to guide the development of the hospital of the future, hospitals may simply freeze into place the status quo of today.
In order to identify these principles, the Joint Commission appointed an expert Roundtable panel comprising hospital administrative and clinical leaders, as well as experts in technology, healthcare economics, hospital design and patient safety. The Roundtable was charged to evaluate the current health care environment and identify the elements of the future hospital that will position it to play an appropriate role or roles in meeting the needs of patients and public. Among specific issues that were addressed by the Roundtable were socio-economic trends, technology, the physical environment of care, patient-centered care values, ongoing staffing challenges, and the global confluence of these issues and their impact on the hospital of the future.
This white paper represents the culmination of the Roundtables discussions. The proposed principles for guiding future hospital development are summarized below:
Principles to Support Economic Viability:
-
- • Encourage the alignment of hospital measurement and payment systems to meet quality and efficiency-related goals
-
- • Apply process improvement tools to improve efficiency and reduce costs
-
- • Pursue coverage options to ensure patient access to, and affordability of, healthcare services
-
- • Address the disequilibrium between the burdens of general acute hospitals and speciality hospitals in fulfilling the social
- mission for healthcare delivery
Principles to Guide Technology Adoption:
-
- • Establish the business case and sustainable funding sources to support the widespread adoption of health information technology
-
- • Redesign business and care processes in tandem with health information technology to ensure benefit accrual
-
- • Use digital technology to support patient-centered hospital care and extend that care beyond the hospital walls
-
- • Establish reliable authorities to provide technology assessment and investment guidance for hospitals
- • Adopt technologies that are labor-saving and integrative across the hospital.
Principles to Guide Achievement of Patient Centered Care:
-
- • Make adoption of patient-centered care values a priority for improving patient safety and patient and staff satisfaction
-
- • Incorporate patient-centered care principles into the activities of hospital oversight bodies and transparency initiatives
-
- • Address barriers to patient and family engagement, such as low health literacy and personal and cultural preferences
-
- • Eliminate disparities in the quality of care for minorities, the poor, the aged and the mentally ill
- • Improve the quality of care for the chronically ill through adoption of care models that encourage coordinated, multi-disciplinary care
Principles to Address the Staffing Challenge:
-
- • Address the maldistribution of health care workers across the globe by instilling fair migration and compensation policies for affected countries
-
- • Expand health professional education and training capacity to accommodate the growing demand for health care workers
-
- • Create work place cultures that can attract and retain health care workers
-
- • Support the development of health professional knowledge and skills required to care for patients in an increasingly complex environment
-
- • Educate health professionals to deliver team-based care and promote teamwork in the hospital environment
- • Develop the competence of health professionals to acre for geriatric patients
Principles to Guide Design:
-
- • Incorporate evidence-based design principles that improve patient safety, including single rooms, decentralized nurse stations and noise reducing materials, in hospital construction
-
- • Address high-level priorities, such as infection control and emergency preparedness in hospital design and construction
-
- • Include clinicians, other staff, patients and families in the design process to maximize opportunities to improve staff work flow and patient safety, and create patient-centered environments
-
- • Design flexibility into the building to allow for better adaptation to the rapid cycle of innovation in medicine and technology
- • Incorporate “green” principles in hospital design and construction
Planning, Design, and Construction of Health Care Facilities,Third Edition
By
The Joint Commission
About This Book
A health care facilities new or improved design establishes the basis for safe and effective care within that structure. Designing and executing a construction or renovation project requires resources, education, communication and collaboration throughout the process. When patient and worker safety are at risk, the stakes for a successful project are even higher.
This third edition of Planning, Design and Construction of Health Care Facilities – developed in conjunction with the American Institute of Architects Academy of Architecture for Health (AIA-AAH) – presents a comprehensive guide for health care organizations around the world looking to build new facilities or update current structures. This revised edition offers the following:
- • New and expanded information on the topics of process improvement, risk assessment, healthcarecommissioning,
designing for safety and reliability, alternate facility delivery models, and much more
- • Case studies that highlight the application of key strategies
Health care organization leaders, their facilities managers, and the architects, designers and construction firms they work with will all benefit from Planning, Design, and Construction of Health Care Facilities, Third Edition. In fact, the AIA-AAH recommends this book as preparation for becoming a certificate holder in the American College of Health Care architects (ACHA). A board certified health care architect with ACHA credentials is the only specialized certification recognized by the AIA.
About Joint Commission Resources
The mission of Joint Commission Resources (JCR) is to continuously improve the safety and quality of health care in the United States and in the international community through the provision of education, publications, consultation, and evaluation services.
About American Institute of Architects Academy of Architecture for Health
The mission of the American Institute of Architects Academy of Architecture for Health (AIA-AAH) is to improve both the quality of health care design and the design of healthy communities by developing, documenting and disseminating knowledge; educating design practitioners and other related constituencies; advancing the practice of architecture; and affiliating and advocating with others that share these priorities.
The Role of the Physical Environment in the Hospital of the 21st Century: A Once-in-a-Lifetime Opportunity
By
Roger Ulrich & Craig Zimring
A visit to a U.S. hospital is dangerous and stressful for patients, families and staff members. Medical errors and hospital acquired infections are among the leading causes of death in the United States, each killing more Americans than AIDS, breast cancer, or automobile accidents (Institute of Medicine, 2000; 2001). According to the Institute of Medicine in its landmark Quality Chasm report: “The frustration levels of both patients and clinicians have probably never been higher. Yet the problems remain. Health care today harms too frequently and routinely fails to deliver its potential benefits” (IOM, 2001). Problems with U.S. healthcare not only influence patients; they impact staff. Registered nurses have a turnover rate averaging 20 percent (Joint Commission on Accreditation of Healthcare organizations, 2002).
At the same time, the United States is facing one of the largest hospital building in US history. As a result of a confluence of the need to replace aging 1970’s hospitals, population shifts in the United States, the greying of the baby boom generation, and the introduction of new technologies, the United States will spend more than $16 billion for hospital construction in 2004, and this will rise to more than $20 billion per year by the end of the decade (Babwin, 2002). These hospitals will remain in place for decades.
This once-in-a lifetime construction program provides an opportunity to rethink hospital design, and especially to consider how improved hospital design can help reduce staff stress and fatigue and increase effectiveness in delivering care, improve patient safety, reduce patient and family stress and improve outcomes and improve overall quality.
Just as medicine has increasingly moved toward “evidence-based medicine,” where clinical choices are informed by research, healthcare design is increasingly guided by rigorous research linking the physical environment of hospitals to patients and staff outcomes and is moving towards “evidence-based design” (Hamilton, 2003). This report assesses the state of the science that links characteristics of the physical setting to patient and staff outcomes.
-
• What can research tell us about “good” and “bad” hospital design?
• Is there compelling scientifically credible evidence that design genuinely impacts staff and clinical outcomes?
• Can improved design make hospitals less risky and stressful for patients, their families, and staff?
In this project, research teams from Texas A&M University and Georgia Tech combed through several thousand scientific articles and identified more than 600 studies – most in top peer-reviewed journals – that establish how hospital design can impact clinical outcomes. The team found scientific studies that document the impact of a range of design characteristics, such as single-rooms versus multi-bed rooms, reduced noise, improved lighting, better ventilation, better ergonomic design, supportive workplaces and improved layout that can help reduce error, reduce stress, improve sleep, reduce pain and drugs, and improve their outcomes. The team discovered that, not only is there a very large body of evidence to guide hospital design, but a very strong one. A growing scientific literature is confirming that the conventional ways that hospitals are designed contributes to stress and danger, or more positively, that this level of risk and stress is unnecessary: improved physical settings can be an important tool in making hospitals safer, more healing, and better places to work.
To Err Is Human: Building A Safer Health System
By
Institute Of Medicine
PrefaceTo Err Is Human: Building A Safer Health System. The title of this report encapsulates its purpose. Human beings, in all lines of work, make errors. Errors can be prevented by designing systems that make it hard for people to do the wrong thing and easy for people to do the right thing. Cars are designed so that drivers cannot start them while in reverse because that prevents accidents. Work schedules for pilots are designed so they don’t fly too many consecutive hours without rest because alertness and performance are compromised.
In health care, building a safer system means designing processes of care to ensure that patients are safe from accidental injury. When agreement has been reached to pursue a course of medical treatment, patients should have the assurance that it will proceed correctly and safely so they have the best chance possible of achieving the desired outcome.
This report describes a serious concern in health care that, if discussed at all, is discussed only behind closed doors. As health care and the system that delivers it become more complex, the opportunities for errors abound. Correcting this will require a concerted effort by the professions, health care organizations, purchasers, consumers, regulators and policy-makers. Traditional clinical boundaries and a culture of blame must be broken down. But most importantly, we must systematically design safety into processes of care.
This report is part of a larger project examining the quality of health care in America and how to achieve a threshold change in quality. The committee has focused its initial attention on quality concerns that fall into the category of medical errors. There are several reasons for this. First, errors are responsible for an immense burden of patient injury, suffering and death. Second, errors in the provision of health services, whether they result in injury or expose the patient to the risk of injury, are events that everyone agrees just shouldn’t happen. Third, errors are readily understandable to the American public. Fourth, there is a sizeable body of knowledge and very successful experiences in other industries to draw upon in tackling the safety problems of the health care industry. Fifth, the health care delivery system is rapidly evolving and undergoing substantial redesign, which may introduce improvements, but also new hazards. Over the next year, the committee will be examining other quality issues, such as problems of overuse and underuse.
At some point in our lives, each of us will probably be a patient in the health care system. It is hoped that this report can serve as a call to action that will illuminate a problem to which we are all vulnerable.
Foreword
This report is the first in a series of reports to be produced by the Quality of Health Care in America project. The Quality of Health Care in America project was initiated by the Institute of Medicine in June 1998 with the charge of developing a strategy that will result in a threshold improvement in quality over the next ten years.
Under the direction of Chairman William C. Richardson, the Quality of Health Care in America Committee is directed to:
- • Review and synthesize findings in the literature pertaining to the quality of care provided in the health care system.
- • Develop a communications strategy for raising the awareness of the general public and key stakeholders of quality care concerns and opportunities for improvement.
- • Articulate a policy framework that will provide positive incentives to improve quality and foster accountability.
- • Identify characteristics and factors that enable or encourage providers, health care organizations, health plans and communities to continuously improve the quality of care.
- • Develop a research agenda in areas of continued uncertainty.
This first report on patient safety addresses a serious issue affecting the quality of health care. Further reports in this series will address other quality-related issues and cover areas such as re-designing the health care delivery system for the 21st century, aligning financial incentives to reward quality care and the critical role of information technology as a tool for measuring and understanding quality. Additional reports will be produced throughout the coming years.
Concepts in Flexibility in Healthcare Facility Planning, Design and Construction
Tannis Chefurka and Faith Nesdoly, Partners, RPG-Resource Planning Group Inc. and John Christie, Director, Parkin Architects
This is an excellent and well thought-out document, if a bit dated, but for Western applications. It is still very relevant to us in India. If you find it difficult to read, kindly try to read and understand only the text highlighted in blue and the comments in red. Even an architect would find the going difficult.
2010 ADA Standards For Accessible Design
(ADA: Americans with Disabilities Act)
Prepared By
The Department of Justice, USA.
Overview
The Department of Justice published revised regulations for Titles II and III of the Americans with Disabilities Act of 1990 “ADA” in the Federal Register on September 15, 2010. These regulations adopted revised, enforceable accessibility standards called the 2010 ADA Standards for Accessible Design “2010 standards” or “Standards”. The 2010 Standards set minimum requirements-both scoping and technical-for newly designed and constructed or altered State and local government facilities, public accommodations, and commercial facilities to be readily accessible to and usabale by individuals with disabilities. Adoption of the 2010 Standards also establishes a revised reference point for Title II entities that choose to make structural changes to existing facilities to meet their program accessibility requirements; and it establishes a similar reference for Title III entities undertaking readily achievable barrier removal. The Department is providing this document with the official 2010 Standards in one publication. The document includes:
- The 2010 Standards for State and local governments, which consist of the Title II regulations at 28 CFR 35.151 and the 2004 ADAAG at 36 CFR part 1191, appendices B and D.
- The 2010 Standards for public accommodations and commercial facilities which consist of the Title III regulations at 28 CFR part 36, subpart D, and the 2004 ADAAG at 36 CFR Part 1191, appendices B and D.
Legalese aside, (which I have provided above as a matter of form), I think a society that cares for its disabled members is a civilized, humane and mature society. Being mentally challenged, I keenly feel the need for legislation to provide for the needs of differently-abled people. I encourage all designers of the built environment to champion this noble and just cause. In India, healthcare architects can make a start by designing healthcare facilities that are handicapped accessible throughout. I hope these standards will be of help.
Planning Hospitals of the Future
By
Richard Sprow, AIA
Over the last 60 years, there have been recurring trends in thinking about the planning and design of hospital facilities, which seem to go through cycles. Specialty hospitals, new standards for patient rooms, ideas for efficient nursing unit planning, and design for healing environments; all have been the subject of architectural thinking in the past and then interest has subsided – but all will certainly be back again. As planners in one of the world’s largest healthcare design practices, we spend every day talking with hospital managers about future planning issues, which are often linked to market responsiveness, new technologies, and changing expectations about healthcare delivery.The Intergalactic Design Guide – Harnessing the Creative Potential of Social Design
By
Cheryl Heller
Social Design is a new kind of leadership. It offers innovative approaches for increasing creativity, strengthening relationships, and developing our capacity to collaborate – with the potential to transform everything from corporate culture to cities. It pushes us to become comfortable with uncertainty, to design ourselves for change. In The Intergalactic Design Guide, business strategist and designer Cheryl Heller explains eleven common principles, a step-by-step process, and essential skills for successful social design. She uses in-depth examples – from the CEO of a multi-national carpet manufacturer to a young entrepreneur with a passion for reducing food waste – to illustrate how applying the social design process brings together innovative elements of business and design. While changemakers like Paul Farmer and Oprah Winfrey have instinctively practiced social design for decades, Heller organizes concepts applied by leaders in diverse fields so that they become accessible to all of us, no matter the focus of our work. From start-ups to global NGO”s. the Intergalactic design guide provides both inspiration and practical steps for designing a more resilient and fulfilling future. Thought leader David Orr wrote, “If our industrial civilization was entered into an intergalactic design competition, it would be tossed out in the qualifying round.” This book points the way for us to change how we relate to our world, and to each other.
About The Author
 CHERYL HELLER has a history of building new capacities within organizations that expand their reach and make them more resilient. She is the Founding Chair of the first MFA program in Design for Social Innovation at SVA, with alums now working as change leaders in industry, government and the social sector. She is the founder of the design consultancy CommonWise and of the MeasuredLab, which she created in 2017 to investigate the impact of social design on human health. She founded the first design department in a major advertising agency and as a strategist, has helped grow businesses divisions and products, reinvigorated moribund cultures, and designed strategies for hundreds of successful entrepreneurs. She has taught creativity to leaders and organizations around the world. Heller is a recipient of the prestigious AIGA Medal for her contribution to the field of design and was recently recognized by the Rockefeller Foundation with a Bellagio Fellowship.
Her clients have included Ford Motor Company, American Express, Reebok, Marriot International, MeadWestIvaco, StoraEnso, the Arnhold Institute for Global Health, Medtronic, Mars Corporation, Discovery Networks International, Heman Miller, Bayer Corporation, Seventh Generation, L’Oreal, Elle Magazine, Harper’s Bazaar, The World Wildlife Fund, Ford Foundation, Lumina Foundation, The Graduate Network and the Girl Scouts of America.
Heller is the former Board Chair of PopTech, and a Senior Fellow at the Babson Social Innovation Lab. She created the Ideas that Matter program for Sappi in 1999, which has since given over $14 million to designers working for the public good, and partnered with Paul Polak and the Cooper Hewitt National design Museum to create the exhibit, “Design for the Other 90%”. She is currently working on a Ph.D. at RMIT University in Melbourne.
CHERYL HELLER has a history of building new capacities within organizations that expand their reach and make them more resilient. She is the Founding Chair of the first MFA program in Design for Social Innovation at SVA, with alums now working as change leaders in industry, government and the social sector. She is the founder of the design consultancy CommonWise and of the MeasuredLab, which she created in 2017 to investigate the impact of social design on human health. She founded the first design department in a major advertising agency and as a strategist, has helped grow businesses divisions and products, reinvigorated moribund cultures, and designed strategies for hundreds of successful entrepreneurs. She has taught creativity to leaders and organizations around the world. Heller is a recipient of the prestigious AIGA Medal for her contribution to the field of design and was recently recognized by the Rockefeller Foundation with a Bellagio Fellowship.
Her clients have included Ford Motor Company, American Express, Reebok, Marriot International, MeadWestIvaco, StoraEnso, the Arnhold Institute for Global Health, Medtronic, Mars Corporation, Discovery Networks International, Heman Miller, Bayer Corporation, Seventh Generation, L’Oreal, Elle Magazine, Harper’s Bazaar, The World Wildlife Fund, Ford Foundation, Lumina Foundation, The Graduate Network and the Girl Scouts of America.
Heller is the former Board Chair of PopTech, and a Senior Fellow at the Babson Social Innovation Lab. She created the Ideas that Matter program for Sappi in 1999, which has since given over $14 million to designers working for the public good, and partnered with Paul Polak and the Cooper Hewitt National design Museum to create the exhibit, “Design for the Other 90%”. She is currently working on a Ph.D. at RMIT University in Melbourne.
The Intergalactic Design Guide – Harnessing the Creative Potential of Social Design by Cheryl Heller is an excellent book, timely and relevant, and a must read for anyone concerned about the issues that face us globally today.
I urge you to buy this book and read it with attention. It is available on Amazon.in at the following link: https://www.amazon.in/Intergalactic-Design-Guide-Harnessing-Potential/dp/1610918819/ref=sr_1_1?crid=3HSXB90CL84A&dchild=1&keywords=the+intergalactic+design+guide+cheryl+heller&qid=1635635991&qsid=259-3332233-5117125&s=books&sprefix=the+intergalactic+design+guide+cheryl+heller%2Cstripbooks%2C212&sr=1-1&sres=1610918819&srpt=ABIS_BOOK
Health Benefits of Gardens in Hospitals
Roger S. Ulrich, Ph.D.
Findings from several studies have converged in indicating that simply viewing certain types of nature and garden scenes significantly ameliorates stress within only five minutes or less. Further, a limited amount of research has found that viewing nature for longer periods not only helps to calm patients, but can also foster improvement in clinical outcomes — such as reducing pain medication intake and shortening hospital stays.Well-designed hospital gardens not only provide restorative and pleasant nature views, but also can reduce stress and improve clinical outcomes through other mechanisms such as increasing access to social support, and providing opportunities for positive escape from stressful clinical settings.
As well, evidence from studies of a number of hospitals strongly suggests that gardens and other nature helps to heighten patient and family satisfaction with the healthcare provider and the overall quality of care. Research has begun to appear suggesting that hospital gardens also increase staff satisfaction with the workplace, and can be advantageous in hiring and retaining qualified personnel. The potential for hospital gardens to improve medical outcomes, satisfaction, and economic outcomes is notably increasing the attention and priority accorded to gardens, as administrators and providers everywhere face strong pressures to increase quality, become more consumer/patient oriented, control costs, and in some locations establish a positive market identify in the face of strong competition from other providers
National Accreditation Board for Hospitals and Healthcare Providers
Accreditation Standards for Hospitals (5th Edition) April 2020 – IndiaForeword
It is my pleasure and pride to release the 5th Edition of Hospital Accreditation Standard of National accreditation Board for Hospitals and Healthcare Providers. Over the years, successive NABH standards have brought about a significant change in the approach taken by the healthcare units in managing and delivering the healthcare services to the patients. NABH standards are accredited by International Society for Quality in Health Care (ISQU). NABH standards focus on patient safety and quality of the delivery of services by the hospitals in the changing healthcare environment. Without being prescriptive, the objective elements remain informative and guide the organization in conducting its operations with focus on patient safety.
This edition has some changes that were incorporated the suggestions made by various stakeholders. For the first time, there are core objective elements related to Patient safety Goals that have to be complied mandatorily irrespective of the compliance to other elements. There are a total of 651 Objective Elements out of which 102 are in the core category which will be mandatorily assessed during each assessment and 30 are in the excellence category which will be assessed during reaccreditation. This will help the healthcare organization in step wise progression to quality system covering the full accreditation cycle. The scoring methodology is changed to a graded system to help recognising even progressive efforts by the organization in implementing the standards. The chapter on Continuous Quality Improvement is now replaced with Patient Safety and Quality to increase the focus on this aspect of healthcare. Each chapter has a bibliography for reference and this will provide organizations a resource for taking quality beyond the requirements of the objective elements.
In view of these, I expect that the healthcare organizations will indeed benefit by the efforts of the technical committee which developed this standard for National accreditation Board for Hospitals and Healthcare Providers.
Dr Atul Mohan Kochhar
CEO, NABH
Neuferts Architects Data – Health
Health Building Note 00-01 – General design guidance for healthcare buildings
Healthcare Architecture Lecture Series 1:
The Planning Grid: Creating A Framework For DesignCirculation: A Critical Issue – Conceptual Clarity, Ease Of Wayfinding & Disability Needs
Designing For Flexibility: Building In Order And Direction For Growth And Change
Healthcare Architecture Lecture Series 2:
Design Concepts: Should Form Always Follow Function?Green Design: Environmentally Effective Design Principles
Alternative Building Forms and Massing: Pros & Cons – Horizontal or Vertical
Healthcare Architecture Lecture Series 3:
The Architecture of Imaging: The Design of the Radiology & Imaging Sciences DepartmentFuture Perfect: Trends Shaping Healthcare Architecture
Equipment Planning: Its Impact on Architectural Design
Plumbing Design for Healthcare Facilities
A Paradigm Shift To Combat Indoor Respiratory Infection
Roadmap To Improve And Ensure Good Indoor Ventilation In The Context Of Covid-19
HVAC Design Manual For Hospitals And Clinics-Second Edition
Health Facility And Equipment Planning And Management
14 Patterns of Biophilic Design
Improving Health & Well-Being in the Built Environment
Whole Building Design Guide
Arup in Healthcare
Arup – Future of Healthcare Ecosystems
Natural Capitalism – Creating the Next Industrial Revolution
Chapter 5 – Building Blocks
A bank whose workers don’t want to go home – A creek that runs through it – green buildings and bright workers – Just rewards and perverse incentives – Windows, light and air – Every building a forecast – Harvesting bananas in the Rockies – Urban forests – Walkable citiesBy: Paul Hawken, Amory Lovins, L. Hunter Lovins.
The world of business is changing – fast. The prevailing model for creating wealth – a model that has its roots in the industrial revolution and that dominated the last century no longer applies. Natural Capitalism introduces an alternative, a new paradigm. Praised by business and political leaders as well as economists and environmentalists around the globe, this ground-breaking book reveals tomorrows most successful global businesses will draw profit from their own environmental responsibility.
“If Adam Smith’s The Wealth of Nations was the bible for the first industrial revolution, then natural capitalism may well prove to be it for the next.”
Peter Senge, author of The Fifth Discipline
“Natural Capitalism is so informative and provocative – and so unfashionably optimistic about the future of the planet – that I wonder why everyone in public life is not reading it and arguing over the implications.”
William Greider, The Nation
“Brimming with examples and anecdotes, Natural Capitalism will exasperate some and excite others – but leave every reader with the hope that the old battle between business and the environment can reach a peaceful and constructive conclusion.”
Frances Cairncross, The Economist
“Natural Capitalism basically proves beyond any argument that there are presently available technologies, and those just on the horizon, which will permit us to get richer by cleaning, not by spoiling, the environment.”
President Bill Clinton
“The message is both huge and simple: The Industrial revolution is over…Natural Capitalism for the most part hangs out a big welcome sign, inviting the reader to step inside and enjoy a cheaper, easier, less-polluting and more energy efficient way to live.”
Christine Colasurdo, San Francisco Chronicle
Paul Hawken, founder of the highly successful gardening supply store Smith & Hawken, recorded his entrepreneurial experiences in the popular book and PBS TV series Growing a Business. He is also the author of The Ecology of Commerce.
Amory and L. Hunter Lovins are the founders of Rocky Mountain Institute, a non-profit resource policy centre. Their efficiency innovations have won major awards around the world.
——————————————————————————————————
The below extract is from the book “Natural Capitalism: Creating the Next Industrial Revolution” and is Chapter 5 “Building Blocks” by Paul Hawken, Amory Lovins and L. Hunter Lovins and is presented here for my architect readers. This very good book is available on Amazon.in at a reasonable price.
Architectural Design and Ethics: Tools for Survival
By Thomas Fisher: Chapter 3 – Why having less is more
In the Scheme of Things: Alternative Thinking on the Practice of Architecture
by Thomas R. Fisher – ExtractsThe Value and Values of Architecture
As architects, our inability to prove our value or articulate our values has a lot to do with the marginalization of the profession, yet the addressing of values is the very stuff of architecture.
The Redesign of Practice
By defining both design and practice in the narrowest terms, we limit the application of our knowledge and the influence of our discipline.
Needed: A Conversation about Ethics
Four classical theories of ethics can be used as a framework to kick off a conversation about some of the dilemmas we face as a profession.
In urban areas in India today, is it not true that the popular image of an architect is that of a pimp for the concerned municipality? When I am introduced as an architect to anyone, I am usually asked one of the following two questions:
1. My upstairs neighbour’s toilet is leaking into mine, what can I do about it?
2. I want to enclose my balcony; can you regularise it for me?
These three essays show us what we can do to improve this sorry situation we as a profession find ourselves in.
Healthcare Resiliency: Seven Ways We Can Design More Resilient Healthcare Projects Today – Stantec
“Primary Protection: Enhancing Health Care Resilience for a Changing Climate”
by Robin Guenther (Perkins + Will, Health Care Without Harm) and John Balbus MD MPH (National Institute of Environmental Health Sciences)Extracts
Part 1: Introduction
Disasters in hospitals do not have to occur to become the subject of intensive planning and programming: future crises and disasters, either more or less similar to previous occasions, or never-before experienced but anticipated occasions, become part of the imagined reality of hospital staff, are considered as having the potential to occur and disrupt the functionality of the hospital, and anticipatory planning and corrective actions take place to respond to them. The planning and mitigation that take place are part of a general culture of mindfulness, a deep-seated awareness that emergencies and accidents are always lurking under the appearance of utter normality, so that disasters, either occurring or imagined, are used by hospital staff as signals of impending trouble which demand their response.
Resilience and Sustainability
Many strategies that are employed to meet sustainable design goals improve resilience. Energy conservation measures, for example, reduce energy demands – a hospital that is less energy intensive can operate longer on a fixed amount of reserve fuel. Medical facilities that reduce their water need can operate longer if they lose water service. Daylit stairwells can be used during daytime hours without need for emergency power. Increasingly, resilience is viewed as the “new sustainable design.”
Health Care’s Response to Extreme Weather
“And, going forward, good design and planning should start with the assumption that nothing will work as intended – or even at all. We should, in other words, take nothing for granted and act as if we have only those within our community and that within our control to depend on…it is the only way to achieve the real optimism of knowing that we can survive, and indeed thrive, regardless of what may happen. We are at out best when we have imagined and accounted for the worst.”
Part 2: The Current State of Health Care Infrastructure Climate Resilience to Extreme Weather Risks
Tropical Cyclones and Hurricanes, Coastal Storms and Surge
…there is growing awareness that hospital campuses must be capable of “island” operation – this is, able to maintain operational capability even when losing municipal electricity, thermal energy, water and sewage utility systems for extended periods of time. Previous policy assumed all necessary services would be restored within 96 hours. Because on-site generators may fail when used at full loads for an extended period of time, coastal hospitals and nursing home facilities are increasingly required to have and electrical re-connection for external mobile generators. The ability to switch quickly from the electrical system to a mobile generator can significantly reduce the likelihood of emergency evacuations during or following a disaster. external generator connections allow the facility to size on-site generators for code-required life safety, critical patient care equipment (those systems that must be able to be operational within 10 seconds of power loss), and critical medical support services; additional mobile generators can be used to handle air conditioning and other systems that can tolerate longer disruption. Prior to a major weather event, external generators can be safely deployed once the event has passed. However, consideration of mobile generators is dependent upon reliable access – such solutions my not be appropriate for barrier islands or locations that could be rendered unreachable by road.
Institution-Level Infrastructure: Assessing Hazards and Vulnerabilities
…hospitals and long-term facilities need to provide secure housing for staff and their families in an extreme weather emergency; this need may drive co-development of hotel facilities or contracts with existing neighbouring hotels than can be activated in emergency planning.
Structural vulnerability considers potential damage to structural components of a building or institution structure. Foundations, bearing walls, columns and beams, staircases, floors and roof decks, or other types of structural components that help support a building are structural components. Applied to site planning, structural components may include roads, vaults or bridges.
The effects of damage to non-structural building components and equipment, as well as the effects of breakdowns in public utility services, communication/IT infrastructure, transportation, re-supply, or other organisational aspects of hospital operations, can be as dangerous to patients as any structural damage.
Ventilation systems are extremely vulnerable to disruption as a result of indirect building damage. Winds often overturn improperly attached roof-mounted ventilation and air-conditioning equipment, while the ductwork is susceptible to collapse once the building enclosure is penetrated. Airborne debris from windstorms or forest fires can quickly clog the air filtration systems, rendering them impaired or inoperable.
Hospitals…depend on several essential pipe systems. Medical gases are among the most important substances that must be channelled through pipes, along with water, steam, and fire-sprinkler systems. Physicians and nurses depend on oxygen and other gases for patient care. Unless properly secured and braced, these installations can be easily dislodged or broken, causing dangerous leakage and potential other damage.
In floods, stormwater management is critical – as rainfall events intensify…roof drainage systems, stormwater retention basins and drywell systems may overflow and cause localized flooding and water damage. Sewers are apt to overflow, backup, or break down. Waste disposal is essential for any residential health care setting, because when the toilets back up, or sterilizers, dishwashers, and other automated cleaning equipment cannot be discharged, patient care is immediately affected. Retention ponds or holding tanks, coupled with backflow and diversion valves, can be employed to solve this problem.
Elevator service is vulnerable not only to power outage, but also to direct damage to elevator installations. Wind and windborne debris can damage elevator penthouses, opening a path for water penetration that can disable elevator motors and controls.
The emergency power supply system is probably the most critical element of a health care system. Together with fuel supply and storage facilities, this system enables all the other hospital installations and equipment that have not yet sustained direct physical damage to function normally in any disaster. As the nature of diagnosis and treatment becomes more dependent on computers, monitors, and other electric equipment, the need for emergency power will continue to grow. Most health care organizations have disaster mitigation or emergency operation plans, but not all of them provide organizational alternatives when the normal daily movement of staff, patients, equipment, and supplies are compromised. The critical nature and interdependence of these processes represent a separate category of vulnerabilities that need careful attention. The disruption of administrative services by natural events can impair hospital functions as much as physical damage.
…the need to safely care for the families of workers during emergencies cannot be underestimated. Hospitals and long-term care facilities must have effective plans to house up to 1000 additional people nearby, out of harm’s way, in buildings that have power, water, and services.
Finally, climate considerations call into question how long emergencies must be managed. Four days, five days – there are stories of facilities that harboured safely in place for more than 100 hours, only to finally need to evacuate due to organizational failures.
It is imperative to recognize the role of front-line health workers, from clinical care to environmental services workers, and the broader community in planning for enhanced organizational resilience. Front-line workers should participate in the development of health care risk assessment and emergency plans, in risk assessment and emergency plans re-evaluations and updates, including lessons learned after specific emergency events.
Transportation systems are potentially vulnerable to the loss of key elements. Therefore, selectively adding redundant infrastructure may be a more efficient strategy than hardening many individual facilities on the existing system. System resilience is best viewed across transportation modes and multiple system owners. While some key elements are obvious, other dependencies may be less well recognized.
Part 3: Solutions for the Future Infrastructure Solutions for Improved Health Care Climate Resilience Key lessons emerge when reviewing post-disaster health care failures and evacuations:
- For critical care health facilities, it may no longer be adequate to depend upon current external community or regionally based mitigation strategies. Hospitals should plan to remain operational even when these larger regional systems fail…. new hospitals in New Orleans are constructed “upside down”: essential medical services and infrastructure are at higher elevations to anticipate a failure of the levee system. Architect Thomas Fisher, in Designing to Avoid Disaster (2013), reminds us that “going forward, good design and planning will be based on the understanding that nothing will work as planned, or even at all.”
- For critical health care facilities, it is no longer acceptable to design new buildings using current disaster thresholds. Planning must recognize that hospitals have a minimum life of 50 years.
- Because recent research and experience suggests that shelter-in-place is the safest long-term option for residential settings, specific infrastructure improvements are required to ensure availability of primary power, emergency power, and water during and following disasters.
- Increasing energy demands at academic health centre campuses, which provide patient care, education, and research facilities, contribute to the growth of on-site power and thermal energy generation as backup to grid supplied energy sources for enhanced reliability and reduced greenhouse gas emissions.
- Duplicative emergency power systems that deliver little to no value during normal, day-to-day operation are less likely to attract adequate investment and maintenance from the private sector.
Personnel responsible for making a health care facility safer for patients, more resistant to damage, or capable of continued operations in a post disaster situation must consider the following questions:
- What types and magnitudes of hazard events are anticipated at the site?
- What are the vulnerabilities of the site or existing building to natural hazards?
- What are the anticipated frequencies of hazard events?
- What level of loss/damage/disruption/injury, if any, is acceptable?
- What might be the financial impact of extended downtime on the institution?
- What is the impact to the community if the hospital cannot maintain operations in the aftermath of a disaster?
This section examines new and emergent practices that integrate sustainable design strategies and resilience thinking in 21st century health care building infrastructure.
Framework for Climate Resilient Health Care Settings The five elements of climate resilient health care infrastructure from the basis for exploring a facility or campuses responses to the challenges of climate change and extreme weather:
- 1.Multi-hazard Assessment-Understanding Climate risk.
- 2.Land Use Planning, Building Design and Regulation
- 3.Infrastructure Protection and Resilience
- 4.Protect Vital Facilities and Functions: Clinical Care and Personnel
- 5.Environmental Protection and Strengthening of Ecosystems
It is understood that these five elements are nested within a broader framework that begins with institutional and administrative support for broader disaster or emergency preparedness efforts, and includes education and training as well as disaster response, recovery and rebuilding, all of which are outside the scope of this Guide.
Element 1: Multi-Hazard Assessment: Understanding Climate Risks and Community Vulnerabilities Maintain up-to-date data on climate hazards and infrastructure vulnerabilities, prepare risk assessments and use these to inform infrastructure planning and decisions. Keep a well-maintained database of disaster losses. The basic components of climate risk assessment include:
- Historic loss data: Consult or maintain an updated database of extreme weather losses from past events on your campus, city or region.
- Hazard assessment: Establish and map the intensity and probability of extreme weather events.
- Capacity assessment: identify the capacities and resources available within your organization, neighbourhood or community to provide redundancy in order to enhance resilience.
- Community vulnerability assessment: Identify the degree of vulnerability and exposures to hazards your community may face, and the likely impact of that vulnerability on both medical services (patient surge) and non-traditional needs (beyond clinical care) the community may expect a medical facility to provide.
- Campus vulnerability assessment: Determine the degree of vulnerability and exposure to the hazard your campus or building(s) may face.
The aim should be to anticipate and coordinate how the building and its systems interact, how mitigation of risk from one hazard can influence the building’s vulnerability to others, and how undesirable conditions and conflicts may be avoided or resolved. Through the application of a multi-hazard and multi-disciplinary approach, cost savings, efficiency, and better performance can be achieved in programming and planning new buildings and retrofitting existing ones.
Case Study: Spaulding Rehabilitation Hospital, Boston, MA
In 2005, Partners Healthcare purchased a contaminated brownfield parcel of land in the Charleston Navy Yard to replace their Spaulding rehabilitation facility. When Hurricane Katrina devastated the healthcare infrastructure in the Gulf region, Partners recognized their potential vulnerability and created a set of voluntary best-practice requirements for the new Spaulding Rehabilitation Hospital, which opened in 2013. This facility is the first building on the Boston waterfront to design for a projected sea level rise.
Key decisions included:
- Placing the First-Floor elevation 30” above the projected 500-year flood elevation, while maintaining universal access for rehabilitation patients.
- Placing all critical patient care functions above the first floor.
- Ensuring a high-performance envelope, including triple glazed windows and exterior shading, to improve thermal performance and prevent low interior temperatures/freezing if heat is lost in winter months or ventilation is inoperable in summer months.
- Incorporating key-operable windows in patient rooms, so that if the building cooling or ventilation system is inoperable, indoor overheating can be avoided in summer months and patients can shelter-in-place.
- Placing all critical mechanical/electrical infrastructure on the roof and above flood elevations, to minimize possibility of interruption.
- Implementing gas-fired on-site cogeneration (CHP) to provide efficiency and redundancy for power generation in the event of grid loss or diesel generator issues (CHP infrastructure is on the roof, as are emergency diesel generators).
- Implementing extensive green roofs to mitigate stormwater discharge during heavy rainfalls.
None of these measures, which collectively added between 0.3 and 0.5 percent to the initial cost of construction, was mandated by federal, state, or local codes. In fact, Partners had to overcome substantial utility resistance to locating cogeneration and major electrical switchgear above the ground floor. In addition to providing enhanced resilience to extreme weather, the building envelope and energy conservation measures reduce energy in normal operation, in turn reducing carbon emissions. The ongoing operational savings from these envelope and system measures more than offset the additional capital investment.
Element 2: Land Use Planning, Building Design, and Regulation
Land use decision making affects the resilience of a campus or building….there is the matter of how and under what set of regulations, buildings have been constructed. Recent extreme weather events suggest that relying on historical baselines will not ensure future building performance. Sustainable design has radically transformed approaches to land use at the individual site and building level, producing approaches that will likely improve resilience to extreme weather events. Many of these strategies are equally appropriate for retrofitting and new development. Orientation of the building can affect the thermal and wind performance of the envelope. Orienting buildings to minimize thermal loads, particularly heat loads, will reduce the probability of overheating if a building’s air conditioning systems fail. In climates dominated by heat, exterior solar shading devices can reduce extremes of solar gain. In such climates, consideration of covered parking also becomes more critical. New hospital construction…anticipates the need to receive personnel, supplies and the injured during extended periods of floodwater inundation. These new hospitals include boat docks and launches at upper levels. Hospital campuses have been significantly hampered by travel disruptions and restrictions following extreme weather events. Access to gasoline, restricted access on bridges and disruptions to major public transit systems have caused lingering access issues for hospitals. For existing health care campuses, it is important to understand the codes that were in place when buildings were constructed, while for new campuses, it is imperative to compare future climate risk projections to current local codes. Because building enclosure failures have been a common occurrence in high wind and flooding events, understanding the vulnerabilities of existing enclosures and developing a plan to harden those enclosures is an important aspect of climate resilience.
Key practices for addressing wind vulnerabilities include:
- Properly anchoring roofing and rooftop equipment in high wind areas (in many instances, roofs and equipment are blown off, leading to water penetration and evacuation of buildings.)
- Removing all items that may become projectiles e.g., Loose furniture and equipment, ballasted (gravel) roofs within 1500 feet of critical buildings
- Designing enclosures to resist high wind and impact resistant glazing and façade construction.
Vertical transportation systems are also vulnerable to flooding and wind damage. High winds can damage rooftop penthouses containing elevator machine rooms; elevator pits are prone to flooding, which disables elevators. While elevators are included as part of the emergency power systems, physical damage may render them useless in emergencies.
Element 3: Infrastructure Protection and Resilience
In general, a CHP system that runs consistently throughout the year is more reliable in an emergency than a backup generator system that only runs during emergencies. Because it is relied upon daily for needed energy services, a CHP system is also more likely to be properly maintained, operated by trained staff, and to have a steady supply of fuel.
For many hospital owners, this shift to CHP is significantly contributing to greenhouse gas emissions and is a cornerstone of voluntary climate commitments.
On-site renewable energy systems provide enhanced resilience. Many US hospitals are installing wind or solar energy systems for both thermal energy (domestic hot water heating) and electric power generation. To date, the performance of renewable energy systems in extreme weather events has been good, with limited damage to such systems from high winds or flooding.
Consistent access to a reliable potable water supply is another key element of resilience. One of the key challenges with fixed quantity emergency water supplies is accurately estimating demand – clearly, the lower the potable water demand, the longer a given supply of water will last. Many hospitals and nursing homes have not historically tracked water usage; there are few reliable benchmarks for water consumption.
Water conservation measures such as low flow fixtures, reduce potable water demand in sanitary fixtures by as much as 40%. Cooling towers for air conditioning systems can consume as much as 50% of the total potable water demand; increasingly, hospitals and nursing homes are shifting to non-potable water sources for such process uses, including captured condensate form air handling units, and rainwater harvesting. In order to meet the requirements for adequate water during municipal disruptions, hospitals and nursing homes may install independent well water services. At the same time, independent water services may have reliability and quality challenges.
Extreme weather events may compromise local water supply quality; if contamination is a risk, fixed potable water storage may be the best option.
In flood situations, all plumbing fixtures connected to the potable water system may become weak points in the system if they allow floodwaters to contaminate the system. Rising floodwaters may force untreated sewage to back up through toilets or floor drains. Specially designed devices that prevent backflow can be installed. On-site wastewater treatment facilities provide an added measure of resilience.
Element 4: Protect Vital Clinical Care Facilities and Functions
Health care facilities, in emergencies, are responsible for more than sheltering residents in place – they are often called upon to deliver medical services to large numbers of injured people. It is imperative that hospitals maintain not only operational infrastructure services, but also vital medical care delivery services. Certainly, recent extreme weather events have demonstrated that ground floor emergency departments in flood-prone areas cannot provide reliable care; expensive and necessary diagnostic imaging equipment (often located on the ground floors due to weight and need for proximity to the ED) may also be destroyed or rendered unusable.
Even if vital mechanical and electrical infrastructure is out of harm’s way, medical care delivery – from submerged departments to corridors connecting egress and transfer pathways – can be severely hampered. Surges of patients often follow weather disasters.
Hospitals must also prepare for and stockpile supplies – more supplies than their “just-in-time” system inventories anticipate – to remain operational through extended transportation and supply chain disruption. In extreme weather events, hospitals must house large numbers of workers, their families and even their pets, in order to continue to deliver high-quality, uninterrupted care while cut off from transportation systems and re-supply infrastructure.
There has been a significant shift in the planning for hospitals in flood-prone regions. Emergency departments (Eds) present particular challenges. Generally, these are located at grade to facilitate ambulance and public access. However, in flood prone areas, this often places Eds below design flood elevation (DFE) and at risk. In coastal areas prone to repeated surge and inundation, hospitals are moving their Eds to higher floors and constructing vehicular and ambulance ramps for normal operation. This has an additional resilience benefit: during high water periods, the ramps facilitate boat mooring to deliver patients, staff and emergency supplies.
Element 5: Environmental Protection and Strengthening of Ecosystems
Healthy ecosystems support life and health. Ecosystem services are goods and services of direct or indirect benefit to humans that are produced by ecosystem processes involving the interaction of living elements, such as vegetation and soil organisms, and non-living elements such as bedrock, water and air. The following elements of ecosystem services should be supported:
- Treating water as a resource: Eliminate unnecessary irrigation and harvest rainwater.
- Valuing soils: Improve infiltration, reduce run-off, and filter stormwater.
- Preserving and enhancing vegetative cover and open space: Maintain wildlife corridors, habitat, wetlands, and reduce the development footprint.
“Enhancing the nation’s resilience will not be easy, nor will it be cheap. But the urgency is there and we need to begin the process now in order to build a national ethos that will make the nation safer, stronger, more secure and more sustainable for our children and grandchildren.”
“Current efforts are hampered by a lack of solid information about the benefits, costs, and effectiveness of various adaptation options, by uncertainty about future climate impacts at a scale necessary for decision-making, and by a lack of coordination.”
“…the science, engineering, and emergency management solutions needed to protect these critical infrastructures and to promote continuity of operations already exist. (The goal) is to tap the available potential in this nation to protect the only infrastructure that provides for our health, and is a major piece of the engine that keeps the nation moving.”
“Designing to Avoid Disaster: The Nature of Fracture-Critical Design”
by Thomas Fisher (Dean and Professor of Architecture at the College of Design, University of Minnesota)In Designing to Avoid Disaster, Fisher discusses the context and cultural assumptions that have led to a number of disasters worldwide, describing the nature of fracture-critical thinking on everything from our economy and politics to our educational and infrastructure systems, to the communities, buildings, and products we inhabit and use every day. And he shows how the natural environment and the human population itself have both begun to move on a path toward a fracture-critical collapse that we need to do everything possible to avoid. We designed our way to such disasters and we can design our way out of them, with a number of possible solutions that Fisher provides.
The extract below on has been taken from the book “Designing to Avoid Disaster: The Nature of Fracture-Critical Design” by Thomas Fisher.
I encourage you to buy and read this very good book; it is available on Amazon.in.
Thinking in Systems: A Primer
by Donella H. MeadowsEdited by Diana Wright, Sustainability Institute
A Note from the Author
This book has been distilled out of the wisdom of thirty years of systems modelling and teaching carried out by dozens of creative people, most of them originally based at or influenced by the MIT System Dynamics group. Foremost among them is Jay Forrester, the founder of the group. My particular teachers (and students who have become my teachers) have ben, in addition to Jay: Ed Roberts, Jack Pugh, Dennis Meadows, Hartmut Bossel, Barry Richmond, Peter Senge, John Sterman, and Peter Allen, but I have drawn here from the language, ideas, examples, quotes, books, and lore of a large intellectual community. I express my admiration and gratitude to all its members.
I also have drawn from thinkers in a variety of disciplines, who, as far as I know, never used a computer to simulate a system, but who are natural systems thinkers. They include Gregory Bateson, Kenneth Boulding, Heman Daly, Albert Einstein, garret Hardin, Vaclav Havel, Lewis Mumford, Gunnar Myrdal, E.F. Schumacher, a number of modern corporate executives, and many anonymous sources of ancient wisdom, from Native Americans to the Sufis of the Middle East. Strange bedfellows, but systems thinking transcends disciplines and cultures and, when it is done right, it overarches history as well.
Having spoken of transcendence, I need to acknowledge factionalism as well. Systems analysts use overarching concepts, but they have entirely human personalities, which means they have formed many fractious schools of systems thought. I have used the language and symbols of systems dynamics here, the school in which I was taught. And I present only the core of systems theory here, not the leading edge. I don’t deal with the most abstract theories and am interested in analysis only when I can see how it helps solve real problems. When the abstract end of systems theory does that, which I believe it will some day, another book will have to be written.
Therefore, you should be warned that this book, like all books, is biased and incomplete. There is much, much more to systems thinking than is presented here, for you to discover if you are interested. One of my purposes is to make you interested. Another of my purposes, the main one, is to give you a basic ability to understand and deal with complex systems, even if your formal systems training begins and ends with this book.
-Donella Meadows, 1993
In the years following her role as the lead author of the international bestseller Limits to Growth, Donella Meadows remained at the forefront of environmental and social analysis until her untimely death in 2001. Long anticipated, thinking in Systems is a concise and crucial book offering insight for problem solving on scales ranging from the personal to the global. Edited by the Sustainability Institute’s Diana Wright, this essential primer brings systems thinking out of the realm of computers and equations and into the tangible world, showing readers how to develop the systems-thinking skills that thought leaders across the globe consider critical for 21st-century life.
A woman whose pioneering work in the 1970s still makes front-page news, Donella Meadows was a scientist, author, teacher and farmer widely considered ahead of her time. She was one of the world’s foremost systems analysts, winner of a MacArthur Foundation “genius” award, and Pulitzer Prize-nominee for her long running newspaper column. She died unexpectedly in 2001 as she neared completion of Thinking in Systems. For more information, visit www.ThinkingInSystems.org
When you’re walking along a tricky, curving, unknown, surprising, obstacle-strewn path, you’d be a fool to keep your head down and look just at the next step in front of you. You’d equally be a fool just to peer far ahead and never notice what’s immediately under your feet. You need to be watching both the short and long term – the whole system.
“Thinking in Systems” is required reading for anyone hoping to run a successful company, community or country. Learning how to think in systems is now part of change-agent literacy. And this is the best book of its kind.”
-Hunter Lovins, founder and President, Natural Capital solutions and co-author of Natural Capitalism: Creating the Next Industrial Revolution
“When I read Thinking in Systems I am reminded of the enormity of the gap between systemic thinkers and policy makers. If this book helps narrow the gap, it will be Dana’s greatest contribution.”
-Lester Brown, founder and President, Earth Policy Institution
“The publication of Thinking in Systems is a landmark…This book is destined to shape our understanding of socio-ecological systems in the years to come in much the same way that Silent Spring taught us to understand the nature of ecosystems in the 1960s and 1970s.”
-Oran Young, Professor, Donald Bren School of Environmental science and Management at University of California, Santa Barbara
“Dana Meadows was one of the smartest people I ever knew, able to figure out the sensible answer to almost any problem. This book explains how she thought, and is of immense value to those of us who often wonder what she’d make of some new problem. A classic.”
-Bill McKibben, author of Deep Economy
“This clear, fun to read synthesis will help diverse readers everywhere to grasp and harness how our complex world really works.”
-Amory Lovins, Chairman and Chief Scientist, Rocky Mountain Institute
The extract below on has been taken from the book “Thinking in Systems by Donella H. Meadows.
I encourage you to buy and read this very good book; it is available on Amazon.in.
Hope Is an Imperative – On Ecological Design – The Design Revolution: Notes for Practitioners
by David W. OrrDesign as a Healing Profession
The design professions are a form of the healing arts, an ideal with roots again in Vitruvius’s advice that architects ought to pay close attention to sunlight, the purity of water, air movements, and the effects of the building site on human health. The word healing has a close affinity with other words such as holy and wholeness. A larger sense of the profession of architecture, which architect Thomas Fisher deems a “calling,” would aim for the kind of wholeness that creates not just buildings but integral homes and communities. Compare, for example, the idea that “architecture applies only to buildings designed with a view to aesthetic appeal” with architecture defined as “the art of place-making” and creation of “healing places”. In the former sense, design changes with trends in fashionable forms and materials. It is often indifferent to place, people, and time. The goal is to make monumental, novel and photogenic buildings and landscapes that often express only the ego and power of the designer and owner. In contrast, the making of healing places signals a larger allegiance to place that means, in turn, a commitment to the health of other places. Place making is an art and science disciplined by locality, culture, and ecology requiring detailed knowledge of local requirements, weather, topography, and the nature of particular places and a creative dialogue between past, present, and future possibilities. It is slow work in the same way that carefulness has a different clock-speed than carelessness. Place making uses local resources, thereby buffering local communities from the ups and downs of the global economy, unemployment, and resource shortages.
Practiced as a healing art, architecture, for example, would result in buildings and communities that would not compromise the health of people and places. Architects would aim to design buildings and neighbourhoods in which community and conviviality could thrive. At larger scales the challenge is to extend healing to urban ecologies. Half of humankind now lives in urban areas, a percentage that will rise in coming decades to perhaps 80 percent. Cities built in the industrial model to accommodate the automobile are widely recognized as human, ecological, and, increasingly, economic disasters. Given a choice, people abandon such places in droves. But we have good examples of cities as diverse as Copenhagen, Chattanooga, and Curitiba that have taken charge of their futures to create livable, vital, and prosperous urban places – what Peter Hall and Colin Ward have called “sociable cities.” In order to do that, however, designers must see work as fitting in a larger human and ecological tapestry.
As a healing art, ecological design aims towards harmony, which is the proper relation of parts to the whole. Is there a design equivalent to the Hippocratic oath in medicine that has informed medical ethics for two millennia? Are there things designers should not design? What would it mean for designers to “do no harm”?
Looking ahead, the challenge to the design professions is to join ecology and design in order to create buildings, communities, cities, landscapes, farms, industries, and entire economies that accrue natural capital and are powered by current sunlight – perhaps, one day, having no net ecological footprint. The standard is that of the healthy, regenerative ecosystem. In the years ahead we will discover a great deal that is new and rediscover the value of vernacular traditions such as front porches, village squares, urban parks, corner pubs, bicycles, pedestrian-scaled communities, small and winding streets, local stores, riparian corridors, urban farms and wild areas, and well-used landscapes.
Design practiced as a healing art is not a panacea for the failures of the industrial age. However well designed, a world of 7 to 10 billion human beings with unlimited material aspirations will sooner or later overwhelm the carrying capacity of natural systems as well as our own management abilities. There is considerable evidence that humans already exceed the limits of many natural systems. Further, ecological design does not require building; often the best design choices require adaptive reuse or more intense and creative uses of existing infrastructure. Sometimes it means doing nothing at all, a choice that requires a clearer and wiser distinction between our needs and our wants.
What ecological designers can do, and all they can do, is to help reduce our ecological impacts and buy us time to reckon with the deeper sources of our problems, which have to do with age-old questions about how we relate to each other across the boundaries and sometimes chasms of gender, ethnicity, nationality, culture, and time and how we fit into the larger community of life. Ecological design, as a healing art, is a necessary but sufficient part of a larger strategy of healing, health, and wholeness, which brings me to the soul of the matter.
Design for Spirit
For designers it is significant that humans are inescapably spiritual beings, if only intermittently religious. Our choice is not whether we are spiritual or not but whether our spiritual energy is directed to authentic purposes or not. But much of the modern world, however, has been assembled as if people were machines without deeper needs for order, pattern and roots. Modern designers filled the world with buildings and development divorced from their context, existing as if in some alien realm disconnected from ecology, history, culture, people and place. Ecological design, on the other hand, is a process by which we grow into a particular place, becoming citizens of the life-community in that place. It is a process by which dwellings and landscapes and the uses we make of them become part of a larger story. As a kind of storytelling, design is a celebration of the life that connects us with the nature of the places in which we live and work and grounds us in the still larger story of the human journey.
Ecological design is not a formula but rather a complex process of adapting human intentions to ecological realities. It is art as much as science, ethics as much as economics, ecology as much as engineering. And it is a messy, uncertain, difficult, sometimes contentious process demanding a high order of competence, creativity, and goodwill. Properly done, it changes routines of institutional decision making and management. Rules of finance and budgeting, for example, that worked in the industrial era, when the natural capital of soils, forests, water, and climate stability was assumed to be free, no longer do so. Designing ecologically requires the integration of expertise across many disciplines, perspectives and professions, such as energy specialists, ecological engineers, materials scientists, lighting consultants, ecologically adept landscape architects, and engineers who understand buildings as whole systems, and those who will live and work there.
Finally, beyond performance of the obvious functions such as durable shelter, usefulness, and beauty, what more do we want from our buildings, landscapes, and communities? We should want our buildings, neighbourhoods, communities, and cities to honour the ecologies and cultures of the places in which they are built. They should promote rootedness, not anomie. They ought to foster an awareness of connections and ecological competence. They ought to make us smarter and more competent people, not dumb us down. They ought to be designed to regenerate natural capital of soils, trees and biological diversity. They ought to foster possibilities for real human engagement. They ought to be paid for fairly and not offload costs on others. But these, too, are means to still larger ends.
The extract below on has been taken from the book “Hope is an Imperative: The Essential David Orr” by David W. Orr. I encourage you to buy and read this very good book; it is available on Amazon.in.
National Disaster Management Guidelines: Hospital Safety
National Disaster Management Authority – Government of India – 2016The guidelines on Hospital Safety have been developed with the vision that all hospitals in India will be structurally and functionally safer from disasters, such that the risks to human life and infrastructure are minimized.
The overall aim of the guidelines is to mainstream disaster prevention, mitigation, preparedness and response activities into the health sector in our country, with specific focus on hospitals; such that hospitals are not just better prepared but fully functional immediately after disasters and are able to respond without any delay to the medical requirements of the affected community.
The first chapter introduces the need and importance of hospital safety and risk resilience in today’s times. The second chapter focuses upon the key objectives of the said guidelines as mentioned below:
(1) To address hospital safety through a multi-hazard and inter-disciplinary approach;
(2) To ensure structural safety of hospitals (especially of critical facilities);
(3) To ensure that all professionals involved in the day-to-day operation of hospitals are prepared to respond to disasters; and,
(4) To ensure that every hospital in the country has a fully functional and regularly tested Hospital Disaster Management Plan
The third chapter deals with awareness generation activities for hospital safety with an aim to sensitize the key stakeholders and community on the need for disaster management in health facilities and to achieve the overall aim of protecting the lives of patients and health workers by ensuring the structural resilience of health facilities as well as improving the risk reduction capacity of health workers and institutions.
The fourth chapter on hospital preparedness and response focuses upon provisions required to be put in place to ensure functional safety of hospitals/health facilities in disaster situations. The provisions laid down are the minimum required standards that shall be adhered to by all healthcare facilities; and address both internal and external disasters that are likely to affect hospitals. The chapter lays stress upon the key objective of disaster preparedness and response for hospitals/healthcare institutions which is to ensure that they can remain functional and continue providing the necessary health care services during and immediately after an emergency.
The fifth and sixth chapter focus upon the structural and design safety elements as well as fire safety pertaining to hospital. The seventh chapter throws light on the elements pertaining to regular maintenance and inspection for hospitals. The eight chapter provides an overview of the standard Licensing and Accreditation requirements that shall be followed by hospitals to ensure disaster preparedness. Conscious efforts need to be made to achieve the goal of ‘safer and functional hospitals’ in the country at the earliest; and towards this end, the ninth chapter lays down the ‘National Action Framework for Hospital Safety’, as a focused strategy which should be followed to achieve this goal.
This guideline has been formulated to ensure that when implemented at all levels, the risks to human life and infrastructure are minimised; and hospitals are not only better prepared but are optimally functional immediately after disastrous events, such that they are able to respond immediately to the medical requirements of the affected community.
It is strongly recommended that the interventions suggested in this guideline are approached and implemented in a systematic and time bound manner, since disastrous events can happen anytime, anywhere and at any scale.
Sustainable Construction: Green Building Design and Delivery
Charles J. KibertIntegrated Design Process
Although it is true that excellent teamwork is required for any building project, the level of interaction and communication needed to ensure the success of a green building project is significantly higher. Green buildings are a relatively new concept to the industry, and generally it is necessary to orient all members of the project team to the goals and objectives of the project that are related to issues such as resource efficiency, sustainability, certification, and building health, to name a few. This orientation can serve three purposes. First, it can fulfil its primary purpose of informing the project team about all project requirements. Second, it can familiarize the project team with the owner’s priorities for the high-performance green building aspects of the project. Third, it can provide an opportunity to accomplish team building in the form of group exercises for familiarizing the group with the building, the building program, and the building’s green building issues.
Integrated building design or integrated design is the name given to the high levels of collaboration and teamwork that help differentiate a green building design from the design process found in a conventional project. According to the US Department of Energy, integrated design is
[a] process in which multiple disciplines and seemingly unrelated aspects of design are integrated in a manner that permits synergistic benefits to be realized. The goal is to achieve high performance and multiple benefits at a lower cost than the total for all the components combined. This process often includes integrating green design strategies into conventional design criteria for building form, function, performance, and cost. A key to successful integrated building design is the participation of people from different specialities of design: general architecture, HVAC [heating, ventilation, and air conditioning], lighting and electrical, interior design, and landscape design. By working together at key points in the design process, these participants can often identify highly attractive solutions to design needs that would otherwise not be found. In an integrated design approach, the mechanical engineer will calculate energy use and cost very early in the design, informing designers of the energy-use implications of building orientation, configuration, fenestration, mechanical systems, and lighting options.
“Climate Change Resilience In The Built Environment: Principles For Adapting To A Changing Climate”
by World Green Building CouncilWHO Guidelines for Indoor Air Quality: Selected Pollutants
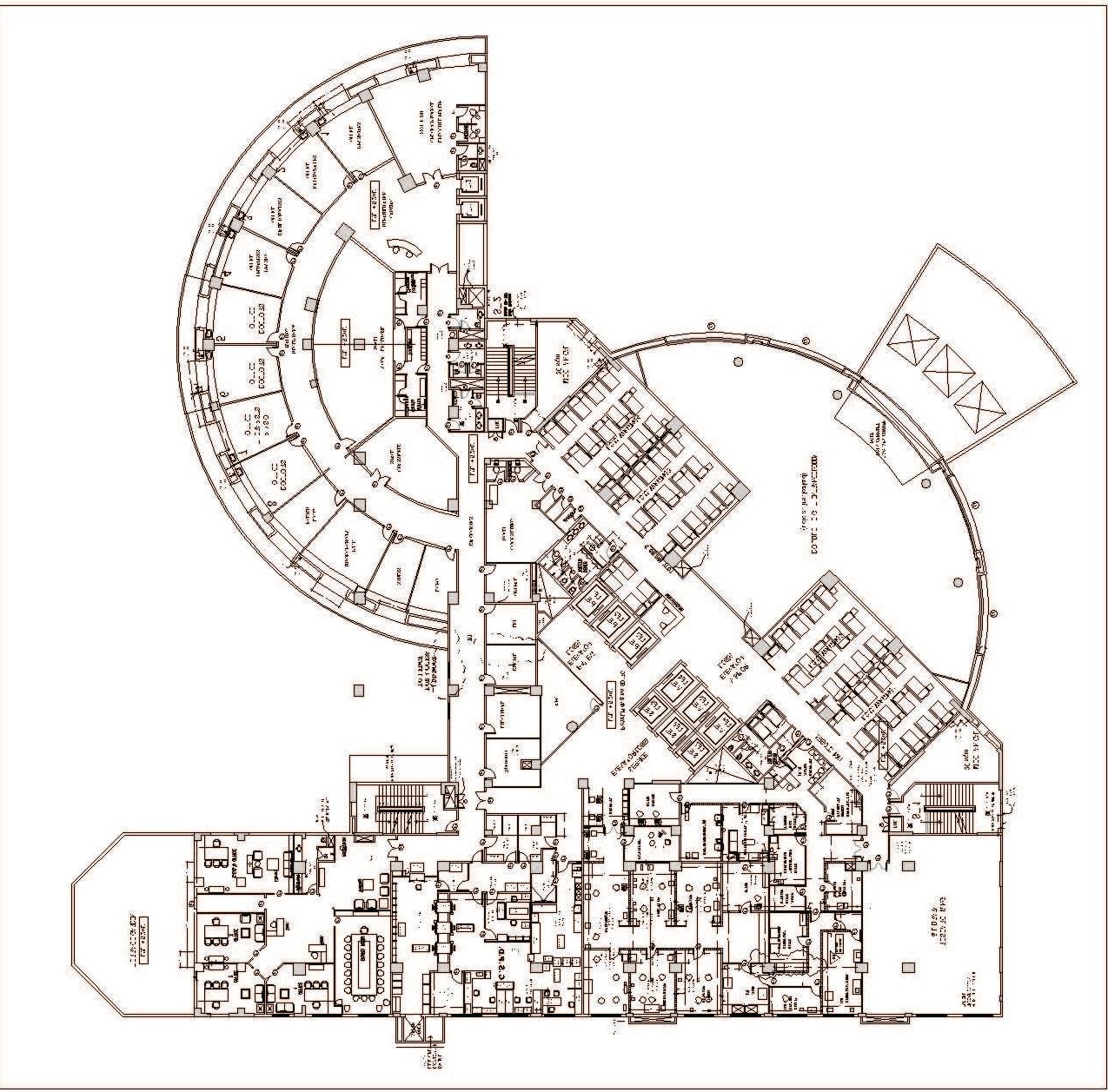
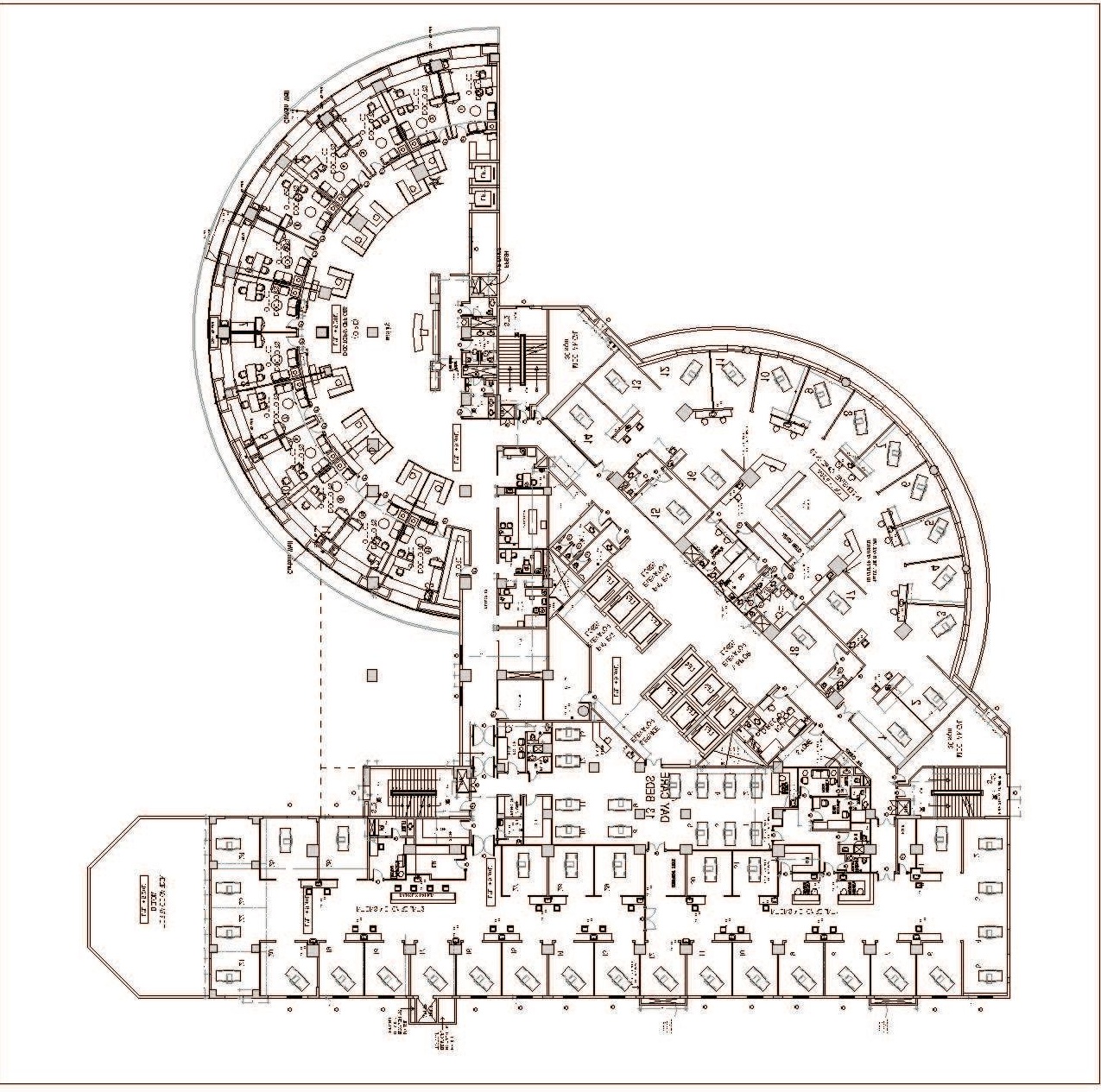
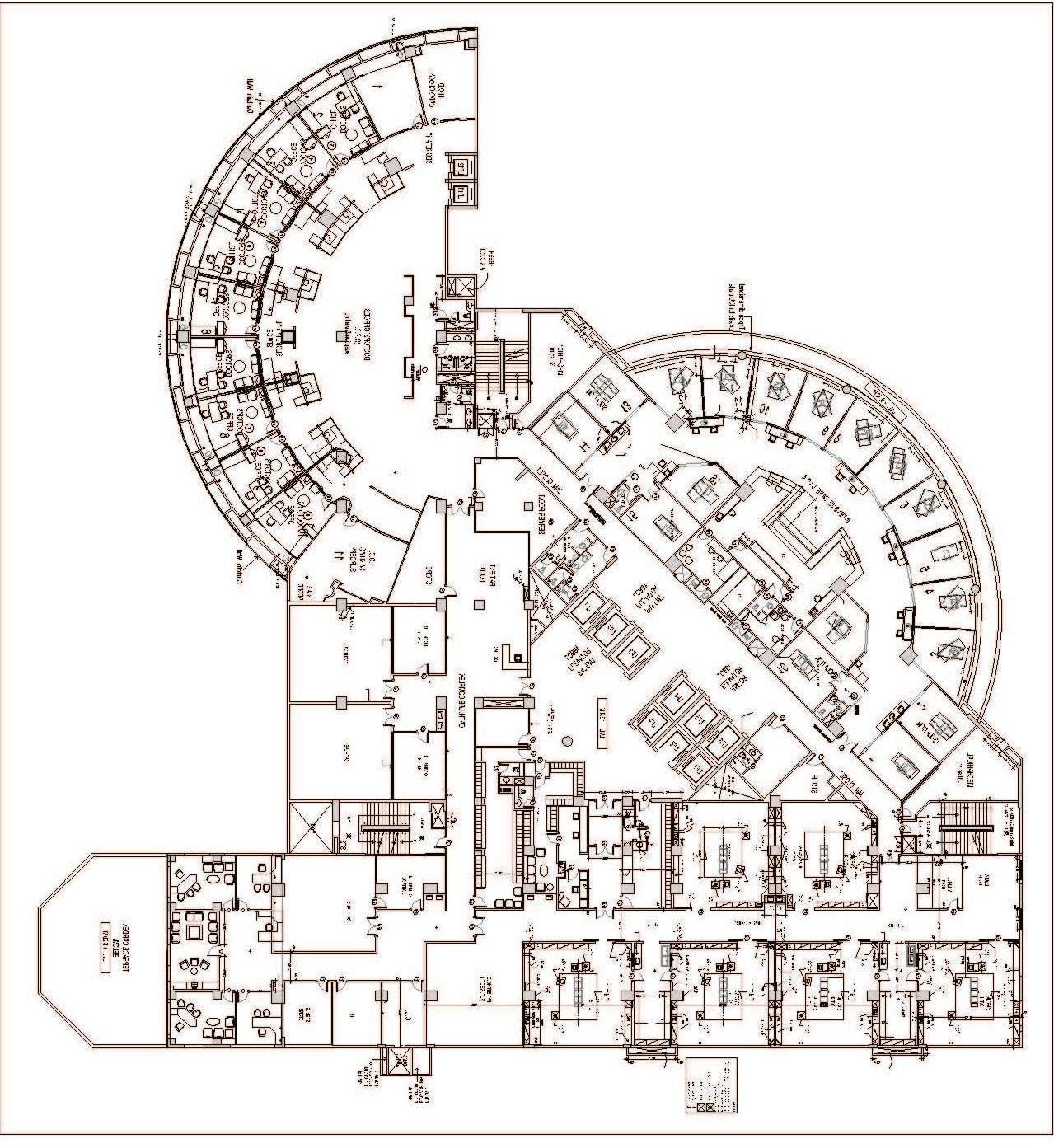

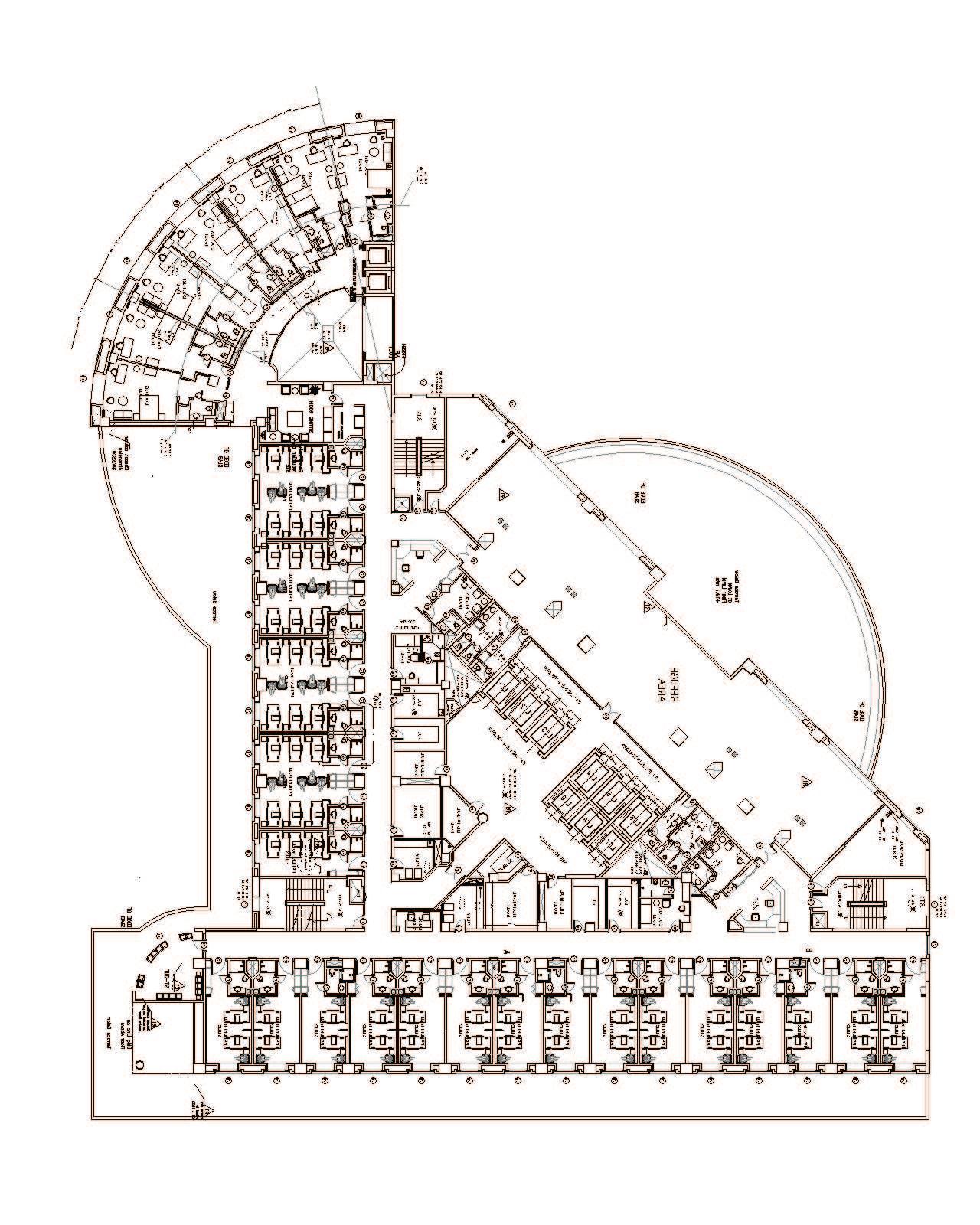




3 thoughts on “About Hussain”