THE SURGICAL SUITE┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā┬Ā
Introduction
Planning for the surgical suite, one of the most important areas of the hospital involves various disciplines. The emotional needs of patients must be catered for and also those of their families. There is no other aspect of hospital care that creates the level of fear and anxiety than surgery. Therefore, any planning process must involve administrators, surgeons, anesthesiologists, surgical nurses, representatives of support areas (housekeeping, pharmacy, central sterile supply, and laboratory) and individuals who consider the needs of the patient and family.
Surgical procedures are performed ion patients for a wide variety of reasons. They may be preformed to correct a potentially life-threatening situation or to provide an improved quality of life. Procedures may be performed in surgical suites that are designed specifically for the treatment of outpatients, such as ambulatory procedure units, or in suites that are designed for┬Ātreatment of both inpatients and outpatients.
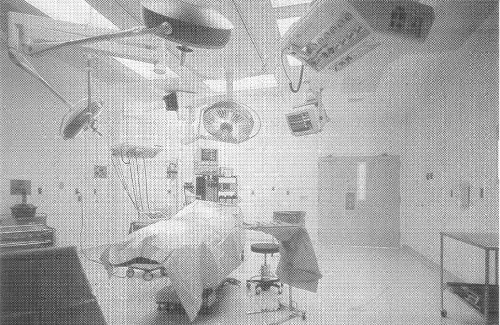 ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬ĀA general operating room at Healthpark Medical center in Fort Myers, Florida.
┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬ĀA general operating room at Healthpark Medical center in Fort Myers, Florida.
Departmental Functions
The function of the department is to receive patients after diagnosis, to anaesthetize them either before or after transfer to the operating table, to operate, and to supervise their post-operative condition before returning them to the wards. The pre-eminent position of the surgical department in the hospital can be appreciated when one realizes that in a typical general hospital, surgical patients represent 50% to 60% of the admissions, and account for an appreciable quantum of the work of and revenue from ancillary departments. The surgical suite of a modern general hospital and everything that goes with it make a very complex workshop. The surgical procedures of the present day, involving more people and highly sophisticated equipment, have rendered ideas of planning of operating rooms of the past somewhat obsolete. The major decision centers on the number and type of operating rooms.
Criteria for Department Sizing
The basic criteria for determining the number of operating rooms are the total number of procedures and number of minutes expected annually for the target year. Calculations are made to determine the total volume of expected surgical operations. The total number of procedures performed in a given period of time is measured against operating room capacity, including procedure and clean-up time. Surgery generally takes place in a seven-to-eight hour, five-day-a-week period beginning at 7.00 A.M. with emergency and some elective surgery occurring during the weekend. When a shortage of operating rooms occurs, it is not uncommon for surgery to take place in the evenings and on weekends.
Composition of the Department
The department consists of one or more operating suites that share ancillary accommodation such as staff changing and rest rooms, arrangements for the reception of patients, and facilities for the disposal of soiled material. The general OTŌĆÖs should have a desirable clear area of 400 sq. ft. (minimum 360 sq. ft.) with 20 ft. clear dimension (minimum 18 ft.) between fixed cabinets and built -in shelves. Rooms for cardio-vascular, orthopedic, neurological, and other special procedures shall have a desirable minimum clear area of 600 sq. ft. (minimum for orthopedic is 360 sq. ft. and for cardiovascular and neurological is 400 sq. ft.), with a desirable clear dimension of 20 ft. (18 ft. for orthopedic). A room for surgical cystoscopic and other endo-urologic procedure should have a desirable area of 350 sq. ft. (minimum 250 sq. ft.) with a clear dimension of 15 ft. The suites may also share a unit for the supply of sterile material and instruments. Each operating suite normally consists of a theater, an anesthesia room, a sterile store and a scrub-up. The orthopedic OT shall have enclosed storage space for splints and traction equipment, which may be outside the OT, but must be conveniently located. The space occupied by the operating rooms is only about one fourth of the surgical suite – the supportive services and functions account for the rest of the space.
Although the requirements of theaters can be met by an entirely internal placement, from the point of view of staff that spend long periods in the department, some natural light can be a valuable asset. This should be provided for some of the ancillary staff rooms. The department should be on a cul-de-sac so that access to it can be strictly controlled (there should be no non-related traffic through the suite). The Intensive Care Unit should be preferably adjacent. X-rays are normally taken with the help of mobile machines. The cleansing and the supply of sterile goods is done in a separate Central Sterile Supply Department (CSSD) that can serve the whole hospital, or a Theater Sterile Supply Unit (TSSU) which can serve a larger number of theaters via a small sterile store attached to each of them.
Flow of various Individuals
Workflow in the surgical suite must be considered in relation to several different groups: patients, visitors, medical staff, nursing staff, and logistical support. Patients enter the suite from inpatient nursing units, the same day surgery area, or emergency. Inpatients generally go to a holding area for surgical preparation, then to their assigned operating rooms. Outpatients are transported to their assigned operating room. After surgery, patients are transported to the PACU for recovery. Next, they go to their assigned patient rooms, or to phase 2 recovery. Visitors wait during surgery in the family waiting area. In some facilities, inpatient family members or visitors wait in the patientsŌĆÖ private room. Outpatient and same day surgery visitors wait in the preoperative waiting area until after the surgery, when a limited number of visitors may be allowed to attend to the patient while he or she is in the phase 2 recovery area.
All surgical staff members change into sterile clothing in dressing areas and enter the surgical suite through a lounge. They can consult the surgery schedule for room assignments. Everyone participating in the surgery scrubs before entering the operating room from the perimeter corridor. After each surgery, the surgeon speaks with the patientŌĆÖs family in a consultation room. Between surgical cases, physicians can take a break in the surgery lounge. There they can utilize the physician dictation areas to record the proceedings/outcome of the surgery.
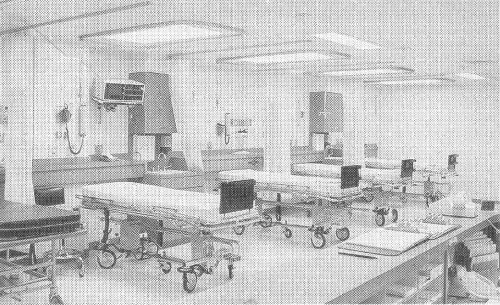 ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā A post-anesthesia recovery room at Duncan Regional Hospital in Duncan, Oklahoma
┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā A post-anesthesia recovery room at Duncan Regional Hospital in Duncan, Oklahoma
 ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬ĀA surgical suite family waiting area at All Saints Episcopal Hospital-Cityview in Fort Worth, Texas
┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬ĀA surgical suite family waiting area at All Saints Episcopal Hospital-Cityview in Fort Worth, Texas
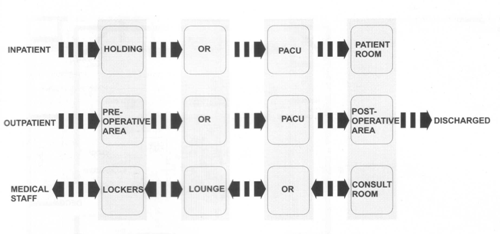 ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā A surgical suite flow diagram
┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā A surgical suite flow diagram
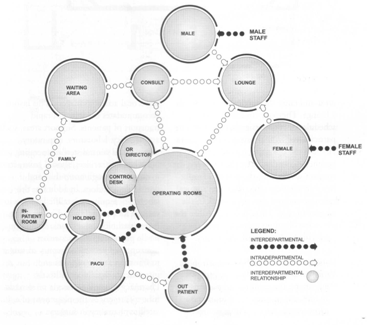 ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā An interrelationship diagram of a surgical suite
┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā An interrelationship diagram of a surgical suite
Reducing Risk of Infection
Of prime importance in the design of the department is the need to reduce to a minimum the risk of infection at the operating table. Ensuring the sterility of instruments and other apparatus is relatively simple, but no less important is the reduction of the risks of airborne infection. This depends upon management procedures and the physical arrangement of the department and of its ventilation system. The physical arrangement should ensure that not only are these procedures facilitated but that as far as possible they are inescapable.
A surgical department could be divided into zones, where the quality of the environment would conform to the cleanliness policy adopted by the individual hospital.
- The general zone – in this zone the requirements for cleanliness correspond to the usual hospital cleanliness standard. This zone includes waiting areas for relatives, catastrophe and triage areas, plaster rooms, offices, record rooms, laboratories, stores for non-sterile material, staff lounge-refreshment rooms, toilets and changing rooms.
- The clean zone – this provides for the surgical department reception and holding area, anesthesia rooms, delivery rooms, endoscopy rooms, stores for blood, medicine, parenteral solutions etc., stores for tubed medical gases, the sterile service area, the general post-anesthesia area, X-ray apparatus stores, and clean bed stores.
- The super clean zone – this accommodates scrub-up and gowning areas, operation theaters, sterile stores, sterile linen stores, and thoracic post-anesthesia rooms.
- The ultra clean zone – is determined by a circle with a one meter diameter from the wound.
- The aseptic zone – is limited to the area of the incision.
To minimize the risk of infection the method of artificial ventilation should ensure that within each suite there is a supply of pure air sufficient to reduce the bacterial count below a critical level. There should be a positive pressure in the theater and sterile store to provide a flow of air from the clean to the less clean areas. Each theater in the department should have its own self-contained ventilation system in order to reduce the risk of cross infection. There should be no movement of air from one suite to another.
For example, the MAQUET VARIOP industrially produced modular operating theater system uses the following system for air-conditioning and air-filtration:
The pre-conditioned and pre-filtered air passes through the distribution ducts of the air-conditioning ceiling to the floating particle filters of classŌĆØH13ŌĆØ. The symmetrical arrangement of the floating particle filters in th
e pressure chamber creates an even distribution of the air volume.
The clean air passes into the room via the special laminar air distributors. Below the ceiling panel, a laminar displacement flow forms. The air exchange in the area below the air intake ceiling is therefore considerably greater than in the rest of the room.
For an even airflow through the room, it is advisable to extract air at four places in the corners of the room at the bottom and top of the wall. Fluff filters are recommended for the lower air extraction intake openings.
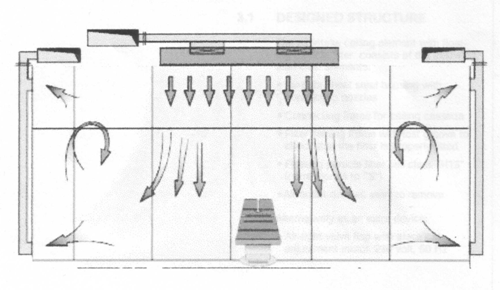 ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬ĀSchematic Diagram of OT Suite Airflow
┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬ĀSchematic Diagram of OT Suite Airflow
Other Area Requirements
A holding area is needed at the entrance of the department where patients are transferred to a theater stretcher. Whether a separate anesthesia room is provided or not, the anesthetist needs a wide variety of equipment, instruments and drugs which calls for considerable storage space. In addition, equipment used in the department, some of them bulky items such as the C-arm and portable X-rays need to be stored in alcoves. After the operation the patient is transferred to a recovery area for recovery from the anesthesia, and then either to his own ward or the ICU. The Post-Anesthetic Care Unit (PACU) (Recovery) area needs to be easily supervised and readily accessible from all the theaters. it should contain a medication station; hand-washing facilities; nurse station with charting facilities; clinical sink; provisions for bedpan cleaning; and storage space for stretchers, supplies and equipment. It would be desirable to have 80 sq. ft. for each bed in addition to the above spaces and a clearance of at least 4 feet between beds and between beds and adjacent walls. The thumb rule for sizing is one and a half to two beds per operating room.
The procedures carried out in the surgical suite are probably the most precise and critical of all the functions performed in a hospital. The suite itself makes the most exacting demands upon detailed design and is frequently the most remote form the average designers direct experience. Ventilation and lighting are probably open to more refined improvement than in any other part of the hospital building. For these reasons there may be much to be said for a design approach that anticipates future flexibility and change instead of attempting precise original design with materials and equipment that may be difficult to alter later.
The following service areas shall be provided:
- A control station located to permit visual observation of all traffic into the suite
- A supervisorŌĆÖs office or station
- A sterilizing facility for immediate or emergency use
- A medication station for distribution of drugs and routine medicine
- An enclosed soiled workroom for the exclusive use of the surgical suite, for the collection and disposal of soiled material
- A clean workroom or clean supply room, where clean materials are assembled prior to use or following the decontamination cycle
- Medical gas storage facilities, in addition to the main storage, separate storage of reserve gas cylinders necessary to complete at least one dayŌĆÖs procedures
- An anesthesia workroom for cleaning, testing and storing anesthesia equipment, with space for anesthesia carts
- An equipment storage room
- Staff clothing change areas, containing lockers, showers and lavatories, and space for donning surgical attire, with a one-way traffic pattern, from ŌĆśdirtyŌĆÖ to ŌĆścleanŌĆÖ.
- Staff lounge and toilet facilities
- Dictation and report preparation areas
- Outpatient recovery
- Change areas for out-patients and same-day admissions
- A space for patient examination, interviews, preparation, testing and obtaining vital signs of patients for out-patient surgery
- Storage areas for portable X-ray equipment, stretchers, fracture tables, warming devices, auxiliary lamps, etc. These areas shall be out of corridors and traffic.
- Housekeeping facilities
- An area for the preparation and examination of frozen sections
- Ice machine
- Provisions for refrigerated blood storage
- Where applicable, appropriate provisions for refrigeration facilities for harvested organs
- Provisions for pathological specimens storage prior to transfer to pathology section
Services, except for the soiled workroom and housekeeping room may be shared with the obstetrical facilities if the functional program reflects this concept. Service areas, when shared with delivery rooms, shall be designed to avoid the passing of patients or staff between the operating room and the delivery room areas.
Operational Relationship
There are several operational issues that affect surgical suite design ŌĆō for example, integrated versus independent outpatient facilities, perimeter work corridor versus interior work core, and integrated versus separate central sterile supply.
The consideration of an integrated versus independent outpatient facility addresses the question of the outpatient service location. Outpatient surgery can be an integrated part of the inpatient surgery suite or separated in an independent outpatient suite that includes both preoperative areas and operating rooms. These areas may be located on or off campus. The appropriate location of this service will involve the medical staff and hospital administration.
A perimeter work corridor layout circles the operating rooms. The layout provides a single corridor system that is used to transport patients, physicians, nursing staff and clean and soiled supplies. Closed clean and soiled case carts and double bagging of waste products are used to maintain sterile conditions. An interior work core separates clean distribution from the soiled distribution system. Placed between two rows of operating rooms, the interior work core is used for sterile supplies and instruments.
The issue of an integrated versus separate central sterile supply (CSS) is whether central sterile supply is placed adjacent to surgery or on another floor: if it is placed directly above or below the surgical suite, it is linked by elevator or dumbwaiter. Although the surgical and CSS staff normally prefer an adjacent relationship, physical building constraints often have a bearing on the location of central sterile supply.
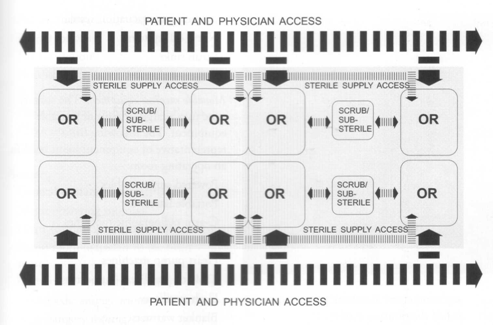
┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬ĀA diagram of a surgical suiteŌĆÖs perimeter corridor concept
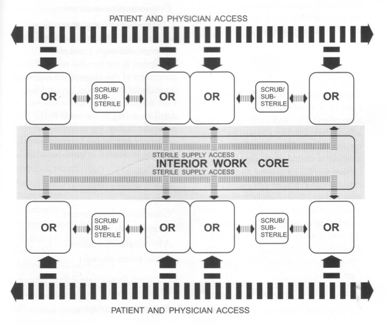
┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā A diagram of a surgical suiteŌĆÖs interior work core concept
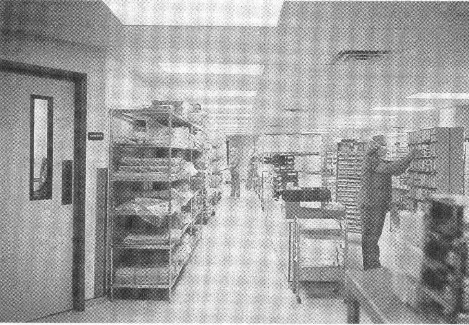 ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā A surgery interior work core at McAllen Regional Medical center in McAllen, Texas
┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā ┬Ā A surgery interior work core at McAllen Regional Medical center in McAllen, Texas
Trends
Surgical facilities will continue to separate outpatient cases from inpatient cases. The trend is, however, toward integrating outpatient with inpatient surgery for greater efficiency in the use of staff and instruments and cost reduction. This trend puts additional pressure on the surgery staff to maintain outpatient standards of care within the inpatient hospital setting. Outpatients will continue to require direct and convenient means of entering the outpatient area.
Pain management services will expand as new and better means of reducing pain are developed. The preoperative patient areas will continue to be key locations for pain management services. The integration of invasive imaging (cath lab) within the surgical suite will increase as a means of delivering invasive imaging in a surgical environment. A developing trend is to combine surgery with magnetic resonance imaging. Each of these trends carries with it the promise of improved surgical services and better care for the patient.
6 thoughts on “Design of a Surgical Suite”